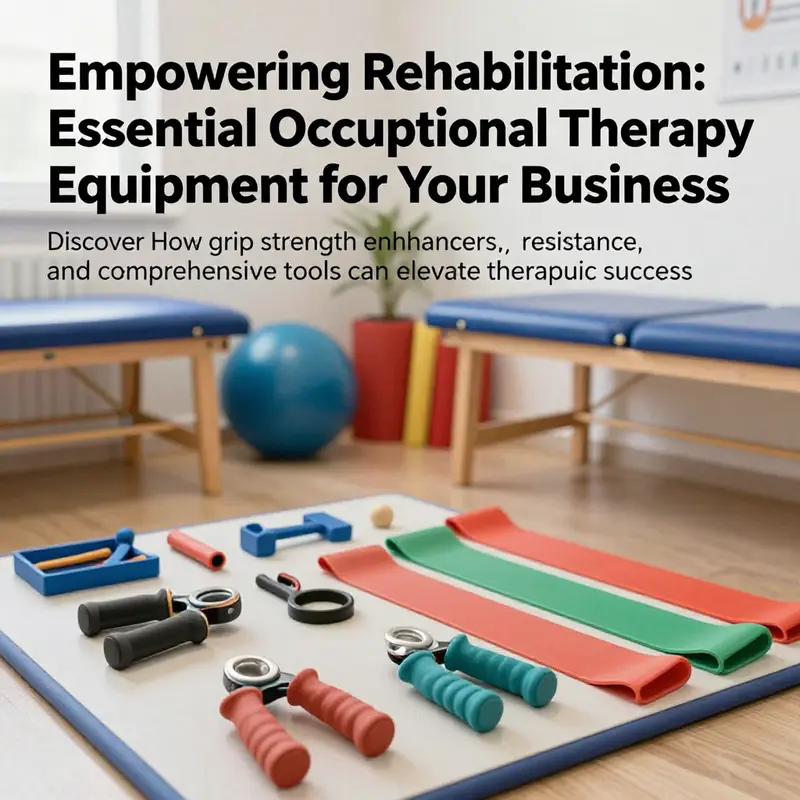
Occupational therapy plays a crucial role in helping individuals reclaim independence following injury or illness. For business owners in this field, understanding the significance of effective occupational therapy equipment is vital for enhancing client outcomes. This article delves into three essential categories of equipment that support therapeutic endeavors. First, we explore grip strength enhancers that aid in building hand dexterity and strength. Following this, we will examine resistance bands, which provide versatile exercise solutions for functional rehabilitation. Lastly, we will discuss comprehensive occupational therapy equipment designed to address diverse rehabilitation needs. By the end, business owners will gain insight into how these tools can help optimize therapy programs and improve the quality of life for their clients.
Grip Strength Tools in Occupational Therapy: Precision, Posture, and Practice
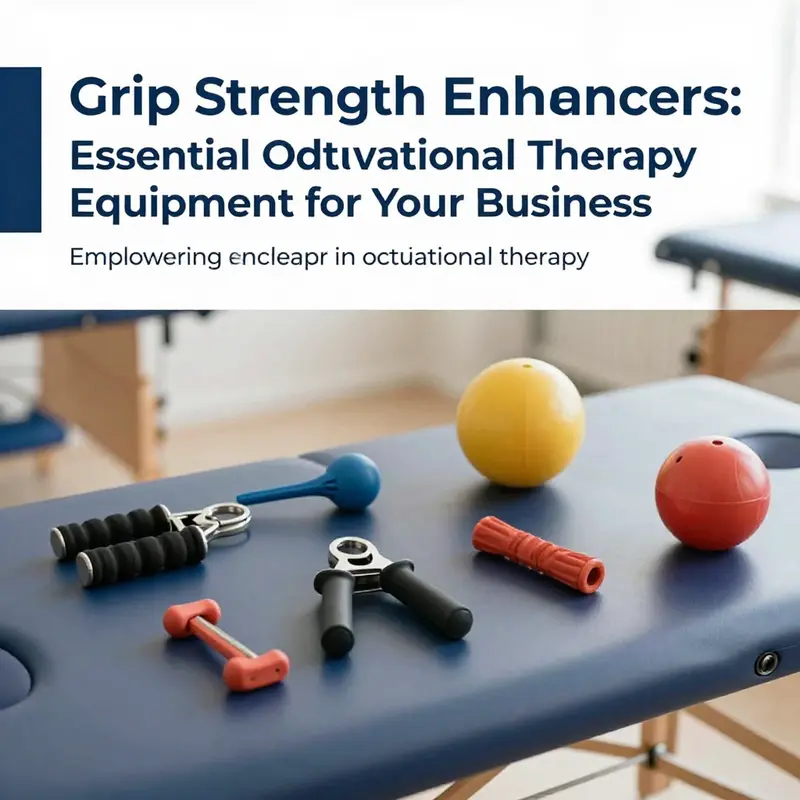
Hand function is a cornerstone of daily independence, and in occupational therapy practice the tools chosen to train grip strength are more than mere gadgets. They are carefully selected instruments that translate therapy into tangible movement, enabling patients to perform tasks that matter in everyday life. The grip strength domain sits at the intersection of motor capacity, sensory feedback, and functional goals. Its equipment—ranging from simple squeeze balls to more refined measurement devices—embodies a philosophy: build stability in the hand, then translate that stability into coordinated action. In many therapy programs, a core set of grip-focused tools forms the backbone of both rehabilitation and prevention, and their value becomes evident when practice is purposeful, progress is measurable, and the patient’s daily routines are gradually redesigned to accommodate regained function. The emphasis on grip is not confined to the rehabilitation clinic; it extends into the home, where consistent, moderate practice can sustain gains and prevent regression. The result is a more autonomous person who can dress, write, prepare meals, and engage with friends and family without frequent assistance. This is why grip strength enhancers occupy a central place in the inventory of occupational therapy equipment and why their use is guided by careful observation, evidence-informed technique, and ongoing data collection.
The spectrum of grip strength tools encompasses devices that apply resistance, provide tactile feedback, or measure force with clinical precision. A common and instructive category is the grip strength ball, a versatile tool designed to elicit targeted activation of the forearm flexors and the intrinsic hand muscles that drive fine motor control. These balls are valued not only for their adjustable resistance—they can be pressed more or less firmly to match a patient’s current capabilities—but also for their capacity to engage the entire upper limb chain. When a patient squeezes, the forearm and wrist work in concert to stabilize the hand, while the fingers respond with graded precision. The central therapeutic message is balance: strength without control is risky, and control without sufficient strength is insufficient for functional tasks. The grip strength ball embodies this balance by providing scalable resistance that can be finely tuned to a patient’s stage of recovery. In stroke rehabilitation, for example, regaining grip involves reactivating neural pathways, reestablishing proprioceptive feedback, and rebuilding endurance to support daily activities such as buttoning a shirt, turning a door handle, or grasping a utensil. For wrist and elbow recovery, correct alignment is essential; therapy literature stresses that the forearm should be in a neutral or near-neutral position to maximize grip efficiency and minimize compensatory movements that could derail progress. In practice, therapists cue patients to maintain a relaxed shoulder, a supported forearm, and a neutral wrist during grip tasks. This posture not only optimizes force generation but also reduces the risk of overuse injuries in the long term. The emphasis on position is not mere instruction; it is a data-informed strategy that shapes how patients perform repetitive tasks over weeks and months, a crucial factor in sustainable rehabilitation outcomes.
Beyond the basic squeeze ball, contemporary OT equipment often includes digital hand dynamometers and related measurement tools that bring a new layer of rigor to grip assessment and progression tracking. The digital hand dynamometer is a medical-grade device capable of recording grip force in kilograms, pounds, or newtons, depending on the protocol and the patient’s needs. The value of these devices lies not only in the accuracy of a single measurement but in the ability to track change over time, identify plateaus, and calibrate resistance with objective criteria. Many digital dynamometers come with memory storage or compatibility with mobile applications, enabling therapists to generate charts that visualize gains to the patient and family members. This data-driven approach supports transparent goal setting, enables shared decision-making, and anchors therapeutic decisions in observable change rather than subjective impression alone. For patients who are preparing to return to regulated work or to more demanding recreational activities, such objective feedback can be a powerful motivator, reinforcing the sense that effort translates into measurable improvement. At the same time, clinicians must preserve a patient-centered lens. The numbers should guide, not dominate; the clinician’s judgment—based on the patient’s overall function, pain levels, fatigue, and daily responsibilities—must harmonize with the readings to tailor a balanced training plan.
The relationship between grip strength tools and broader OT equipment becomes especially clear when we consider how grip-focused work integrates with functional training. An OT gym or clinical therapy setting typically includes a range of devices designed to support balance, coordination, sensory processing, and functional tasks. Platforms that provide stable foot support, adjustable heights, and tactile feedback surfaces may be used to scaffold hand exercises while the patient performs seated tasks such as writing, manipulating small objects, or assembling simple craft activities. Similarly, balance boards or wobble cushions can be incorporated into sessions to challenge postural control as a patient practices grip tasks, promoting dynamic stability that translates to steadier hand movements during daily activities. Sensory integration tools—textures, temperatures, and varying tactile stimuli—can heighten body awareness and improve the patient’s ability to modulate grip force in real time, a skill that is crucial when handling objects of different weights or textures. The integration of these modalities reflects a holistic approach to rehabilitation: strength must be paired with control, endurance with precision, and proprioception with task-specific goals. In this sense, grip strength equipment does not exist in isolation but as a component of a well-orchestrated therapy program designed to restore functional independence across the spectrum of daily life tasks.
Choosing the right equipment and prescribing its use requires the professional judgment of a licensed occupational therapist. Each patient presents a unique constellation of motor, sensory, and cognitive challenges, and the equipment plan must be aligned with individual goals. For some, the priority is to improve the mechanical efficiency of the hand to manipulate small fasteners or utensils; for others, the focus is on sustaining muscle endurance to perform repetitive activities at school, work, or home. The therapist’s assessment guides the progression of resistance, the selection of tools, and the tempo of sessions. A patient with carpal tunnel syndrome, for instance, may benefit from graded resistance within a carefully monitored framework that reduces nerve compression risks while gradually increasing functional grip. A patient recovering from a wrist fracture may require a lighter starting load and slower progression, with frequent reassessment to prevent pain flare-ups or stiffness. Even within the same diagnostic category, differences in age, comorbidities, and daily routines demand a customized approach. The role of digital measurement becomes especially relevant here; data can reveal subtle improvements in grip that are not readily visible through gross observation alone, supporting more nuanced decisions about when to increase load, when to pause, and how to adapt activities to preserve long-term joint health.
Home-based practice represents a critical extension of the therapy plan. The portability and simplicity of grip strength tools make them particularly suitable for home use, where consistent daily practice reinforces gains and helps preserve the gains achieved in clinical sessions. A well-designed home program pairs a modest set of grip devices with clear instructions, visual cues, and a schedule that fits the patient’s lifestyle. The aim is to empower patients to take ownership of their rehabilitation, to recognize the relationship between effort, posture, and outcome, and to develop routines that promote ongoing resilience. When patients experience early successes—such as improved ability to hold a mug without slippage or to turn a key with less effort—the confidence gained can translate into greater willingness to engage in more complex activities. The therapist supports this process by providing feedback on technique during sessions and by reviewing patient-recorded data from any digital devices used in the home setting. This collaborative approach ensures that home practice remains safe, purposeful, and aligned with clinical goals, while also respecting the patient’s preferences, cultural context, and daily responsibilities.
Education about technique and safety is a constant companion to the use of grip strength tools. Proper alignment is essential to maximize power and minimize strain. The forearm should be supported, the wrist maintained in a neutral or near-neutral position, and the elbow typically positioned to keep the shoulder comfortable and free of compensatory movements. In practice, therapists model correct posture, observe micro-movements, and provide real-time feedback as patients perform repetitive squeezes. They also monitor signs of fatigue, pain, or numbness, adjusting the regimen accordingly to avoid exacerbating symptoms. This careful balance—progressing load while safeguarding the patient’s well-being—is a defining feature of high-quality OT care and a key predictor of durable improvement. When patients understand not only how to perform the exercises but why each component matters, they become more adept at integrating these activities into a broader lifestyle strategy that supports ongoing health, resilience, and independence.
The broader implications of grip strength training extend into the measurement of functional capacity, a domain that overlaps with prognosis, return-to-work decisions, and community participation. Grip strength is often used as a proxy for overall upper limb function, and its improvement can influence activity tolerance, manual dexterity, and the execution of daily tasks. Therapists use this information to set realistic, meaningful goals that reflect the patient’s life context. They may plan a progression from single-task exercises to compound activities that require coordination, timing, and sequencing—such as preparing a meal with utensils while carrying a light item in the other hand. In addition, therapeutic decisions may consider the patient’s psychosocial state, motivation, and environmental supports, recognizing that the social and emotional dimensions of recovery are inseparable from physical healing. A patient who gains grip strength but lacks adaptive strategies for environmental obstacles may struggle to translate gains into meaningful autonomy. Therefore, the equipment plan is not merely a numeric endeavor but a narrative about returning to valued activities and re-establishing a sense of control over one’s life.
As grip strength tools continue to evolve, the trend toward digitalization and precision remains pronounced. Sensors, wireless data capture, and app-based feedback systems promise richer, more accessible insights into progress. Yet the core clinical wisdom endures: posture matters, practice must be purposeful, and measurements should be integrated with a holistic view of function, comfort, and safety. The ultimate aim is not to maximize grip force in isolation but to enable reliable, safe, and independent participation in the patient’s daily life. When grip exercises are anchored to real-world tasks, patients perceive the relevance of their therapy more clearly, sustaining engagement and adherence. Therapists, in turn, rely on the convergence of biomechanical knowledge, observational skill, and patient-centered communication to tailor equipment choices and practice plans. The result is a therapy experience that is coherent from the moment a patient enters the clinic to the moment they close the door behind them after a successful day of self-care.
For further reading on the biomechanics underlying grip strength and its clinical implications, see the study that examines forearm position and its impact on grip output. In clinical practice, this evidence informs the precise cues and positioning that make grip training both effective and safe. When a patient learns to align the hand and forearm correctly, the same exercises translate into improved performance in tasks of daily life. In this light, grip strength tools are not merely devices but catalysts for confidence, autonomy, and consistent engagement with one’s own rehabilitation journey. They remind both patient and clinician that progress is a function of technique as much as effort, and that the quiet discipline of daily practice can unlock meaningful change over time.
Internal link: for a broader overview of how specific equipment supports practical therapy in everyday settings, see Tools and Equipment for Occupational Therapists. Tools and Equipment for Occupational Therapists
External reference for deeper biomechanical context: How Forearm Position Affects Grip Strength | American Journal of Occupational Therapy. https://www.ajot.org/doi/10.5014/ajot.2025.796003
Stretching Boundaries: The Quiet Power of Resistance Bands in Occupational Therapy
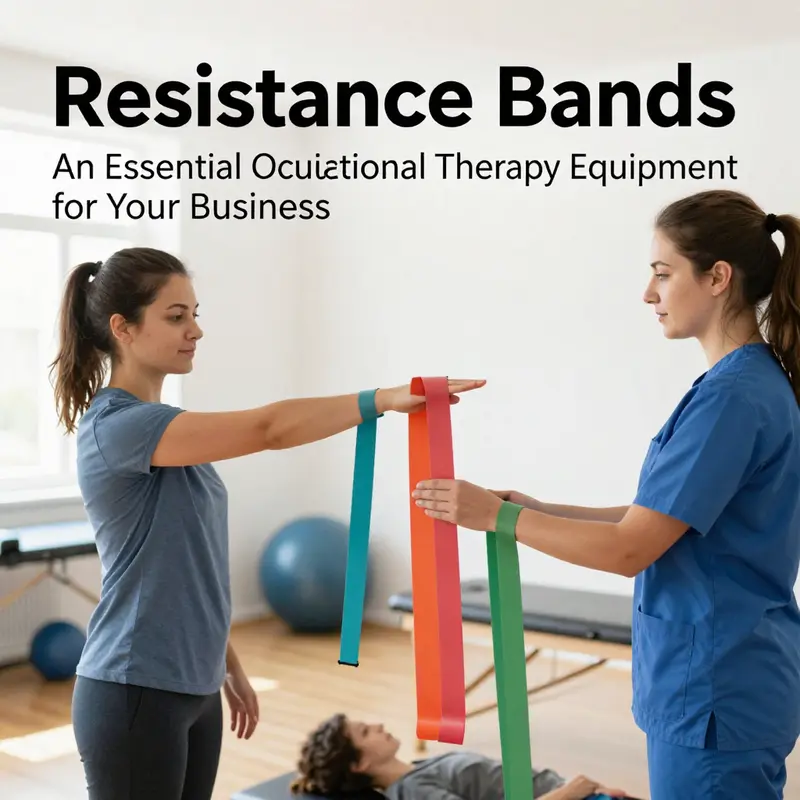
Resistance bands are often overlooked as humble tools, yet in occupational therapy they act like silent partners in the daily rehearsal of movement and independence. They are light enough to carry, adaptable enough to evolve with a patient’s progress, and robust enough to fuse therapeutic intent with real-life tasks. Rather than prescribing a predetermined routine, therapists use resistance bands to sculpt individualized pathways toward functional goals. The bands’ elastic tension can be dialed in with precision, enabling a patient to begin with small, safe challenges and gradually escalate to more demanding tasks that mirror everyday activities such as lifting a dish from a shelf, opening a door, or buttoning a coat. This capacity to tailor resistance makes them especially valuable for clients at different stages of recovery, from the early stages after injury or surgery to the later phases of rehabilitation where endurance, coordination, and motor control are the primary aims.
The essence of resistance bands lies in their adaptability. They accommodate a spectrum of conditions, from arthritis and chronic pain to post-stroke motor planning difficulties and progressive neuromuscular disorders. The low-impact nature of band-assisted exercises protects vulnerable joints while still providing meaningful load. Rather than relying on heavy weights that promote a gravity-dominant form of strengthening, bands offer resistance through a full range of motion, preserving proprioceptive feedback and encouraging controlled eccentric and concentric contractions. When a patient performs a bicep curl with a band, both the lifting and the lowering phases work against tension, reinforcing coordination and muscular endurance in a way that can translate to steadier hand function and steadier grip in daily tasks. This continuous tension also has an effect on neuromuscular control, helping to retrain the timing of muscle firing and the feel of movement as the patient navigates complex hand and forearm tasks.
Clinically, resistance bands shine in their ability to bridge the gap between clinical setting and home practice. A typical OT plan may begin with guided sessions in the clinic to establish form, rhythm, and safety, then gradually shift to a home program that keeps progression within reach. The portability of bands means a patient can carry a compact kit wherever life takes them, ensuring that therapeutic work does not stop when a session ends. The continuity this affords is crucial; repetition in varied contexts strengthens neural pathways and reinforces motor habits that support independence. To therapists, this means more accurate task analysis and better-informed progressions. When prescribing exercises, clinicians consider factors such as the patient’s grip strength, range of motion, scapular stability, and proximal control. They select a band with a resistance level that challenges without overwhelming, and they structure practice to balance effort with rest, allowing for tissue recovery and skill refinement.
From a practical standpoint, the resistance band’s versatility extends beyond simple flexion and extension. Therapists often design sequences that mimic real-world tasks, integrating multi-joint movements that require eye-hand coordination and postural adjustments. A routine may incorporate reaching and grasping a simulated grocery item, stabilizing the trunk while performing a light press, or coordinating breath and rhythm during a resisted shoulder and arm sequence. In this way, the band becomes more than a muscle-building tool; it becomes a vehicle for functional learning. The patient practices not only strength but also control, endurance, and safety habits essential for independent living. As skills improve, therapists layer in more complex activities that fuse sensory input with motor output, supporting both motor planning and sensorimotor integration.
The tactile feedback provided by resistance bands is another aspect that therapists value. The resistance can be altered not only by choosing different bands but also by changing body position or grip, which influences how forces are transmitted through the limb. This feedback helps patients become aware of subtle compensations and prompts real-time correction. For individuals with sensory processing differences, bands offer a controllable, predictable input that can be scaled to meet comfort thresholds. Clinicians can adjust tempo, repetition, and hold times to target specific neural circuits involved in timing and sequencing, which are vital for tasks such as writing, buttoning, or using utensils.
In terms of progression, resistance bands support a thoughtful, data-informed approach to therapy. A progression might begin with isometric holds to establish postural alignment, advance to slow, controlled eccentric loading to build tendon and muscle tolerance, and culminate in dynamic, multi-planar movements that require balance and coordination. The band’s continuous tension means that muscles remain engaged throughout a movement, promoting endurance that is particularly relevant for daily activities like carrying groceries or pushing a wheelchair, where sustained force and control are necessary. This progression is not a matter of piling on volume but of refining timing, control, and confidence. Therapists monitor fatigue, form, and compensatory strategies, using these observations to guide when and how to increase resistance, add complexity, or introduce a new task that resonates with the patient’s personal goals.
Home programs anchored by resistance bands empower clients to take ownership of their rehabilitation. A thoughtfully chosen color-coded system—where bands are labeled by resistance level—can help patients self-regulate their practice. However, the actual practice should be individualized and monitored through periodic re-evaluation rather than a fixed, one-size-fits-all routine. Clinicians often pair the band work with other portable tools, such as small hand therapy putty or finger exercisers, to create a holistic, easy-to-follow regimen that can be performed seated at a kitchen table or standing in a hallway. The key is to align band-based activities with meaningful tasks: folding laundry with steady hands, preparing a meal with controlled grip, or opening a tightly closed container without undue strain. In this sense, resistance bands become a bridge between therapy sessions and the patient’s everyday life.
To support this bridge, therapists frequently reference practical guides and equipment resources that outline how bands can be integrated into comprehensive OT programs. For readers seeking a concise overview of how to select equipment and structure routines, a useful companion resource is available online under the broader topic of Tools and Equipment for Occupational Therapists. That guide provides practical tips on choosing appropriate tools, pairing them with patient needs, and organizing home programs in a way that preserves safety and progress. It is not a substitute for professional judgment, but it offers a tangible starting point for patients and caregivers who want to maintain momentum between sessions. Tools and Equipment for Occupational Therapists
Beyond individual outcomes, resistance bands cultivate a sense of autonomy that many patients find transformative. The ability to perform tasks that once seemed small or inaccessible—gripping a cup securely, turning a doorknob with less tremor, or sustaining a two-minute carry in a kitchen demo—accumulates into a broader sense of capability. Patients begin to anticipate success instead of fearing failure, and this shift can alter daily routines, social participation, and mood. The therapist’s role evolves from merely prescribing activities to coaching patients through a process of self-management. This coaching emphasizes pacing, observable technique, and reflective practice, inviting clients to monitor their own progress, adjust goals, and celebrate small victories along the way.
The clinical value of resistance bands is also echoed in the way they scale to diverse populations. Pediatric clients may use bands to support fine motor control and hand strength within playful activities that resemble everyday tasks, while older adults may benefit from bands that address balance, joint stability, and coordination in a manner that preserves safety and independence. For individuals with neurological conditions, bands can support repetitive, controlled practice necessary for motor relearning and sensory integration. In all cases, therapists remain attentive to safety cues—checking for pain, ensuring comfortable positions, and tailoring resistance to avoid strain while maintaining therapeutic challenge. The aim is not to exhaust but to refine and reinforce, creating a durable base of strength and skill that endures beyond the clinic walls.
As equipment in a therapy gym evolves, resistance bands continue to complement more complex devices like balance boards, stable platforms, and adaptive utensils. The interplay between a stable, controlled resistance and dynamic postural challenges helps patients translate gains from isolated movements into coordinated, functional performance. For example, a patient might practice a shoulder-flexion sequence with a band, then integrate it into a task that requires reaching across a table while maintaining trunk stability. This integrated approach echoes the core OT principle of occupation as therapy: the activity itself is therapeutic because it is meaningful, contextual, and capable of promoting independence. In this sense, resistance bands are not isolated gadgets but versatile partners in a comprehensive rehabilitation strategy.
From the therapist’s perspective, the value of resistance bands lies not only in their immediate effects on strength and control, but also in their ease of integration with documentation and outcome tracking. Clinicians can quantify progress by noting changes in range of motion, hold times, repetition counts, and perceived effort. They can also observe changes in functional performance during real-world tasks and adjust the program accordingly. The practical realities of clinical work—time constraints, patient motivation, and the need for demonstrable progress—are all met by the band’s flexible design. When used thoughtfully, these tools help build a sustainable path toward independence, reducing dependency on caregiver support and enabling individuals to perform daily activities with greater confidence and safety.
In sum, resistance bands embody a powerful blend of simplicity and sophistication. They are light yet robust, affordable yet effective, and portable yet deeply capable of supporting complex rehabilitation goals. They invite patients to engage actively in their recovery while enabling therapists to tailor interventions to unique needs and contexts. The bands’ ability to provide adjustable resistance throughout movement makes them ideally suited to fostering precision, endurance, and functional independence. By bridging clinical practice with home-based practice, resistance bands help ensure that therapy transcends the confines of the clinic and becomes a living, ongoing process of growth and self-efficacy. External resources and professional guidelines reinforce this approach, offering evidence-informed strategies to maximize safety and benefit as patients advance along their rehabilitation journey. For clinicians exploring this tool, the journey is less about mastering a single exercise and more about orchestrating a coherent, patient-centered progression that transforms everyday tasks into reliable, confident actions. External resource: https://www.theraband.com/
Tools of Independence: Comprehensive Occupational Therapy Equipment for Functional Rehabilitation

Occupational therapy equipment serves as the practical backbone of functional rehabilitation. It translates clinical insight into daily gains, supporting skills needed for everyday tasks. Equipment ranges from handheld tools that build grip and dexterity to complex multisensory systems that address cognitive and sensorimotor goals. The aim is reliability, safety, portability, and adaptability so clients can practice in homes, schools, and communities. Selection balances performance and practicality, aligning tools with a client’s goals, environment, and safety considerations. Portable, modular devices support practice outside the clinic and foster consistency in daily routines. Therapists assess strength, range of motion, coordination, and sensory processing to tailor tools that complement rather than fight against a person’s patterns. They also evaluate construction quality and durability to ensure long-lasting use across ages and settings. Common categories include hand-strengtheners, dressing aids, adaptive utensils, reach-and-grasp devices, standing frames, balance equipment, sensory gyms, therapy balls, resistance bands, and weighted tools. Correct technique and progressive challenge, guided by evidence and clinical judgment, help maximize outcomes while preventing fatigue or injury. The therapeutic relationship and caregiver involvement are essential to adapt tools to real-life tasks. In the end, equipment acts as a partner in recovery, growing with the client as goals evolve and settings change.
Final thoughts
Investing in quality occupational therapy equipment is essential for business owners who aim to provide effective rehabilitation services. From grip strength enhancers and resistance bands to comprehensive therapy tools, these assets not only promote functional independence but also empower therapeutic practices. By choosing the right equipment based on client needs and therapy goals, you can greatly enhance rehabilitation experiences and outcomes, fostering a more supportive environment for recovery.