Understanding the differences between physical therapy (PT) and occupational therapy (OT) is critical for business owners in the healthcare sector. Both professions play essential roles in rehabilitation, yet they have distinct objectives and methodologies. This article delves into their respective goals, techniques, and the varied populations they serve. Moreover, we will explore the two fields’ effectiveness in promoting recovery and independence, providing valuable insights for business owners looking to optimize service offerings in their organizations.
How Physical and Occupational Therapy Divide and Combine: Goals, Methods, and Everyday Impact
Physical and occupational therapy share a common mission: to improve a person’s function and quality of life. Yet they approach that mission from different angles. Physical therapy concentrates on restoring movement, strength, balance, and the mechanics of the body. Occupational therapy concentrates on enabling people to carry out the meaningful activities of daily life—dressing, cooking, working, parenting, and social participation. Understanding how these professions differ, overlap, and coordinate helps patients, families, and care teams choose the right interventions at the right time and set realistic, motivating goals.
Both professions begin with a thorough assessment, but what they look for and how they measure success vary. A physical therapist examines range of motion, muscle strength, gait patterns, pain sources, and the nervous system’s role in movement. They test endurance, joint mobility, and balance to design a progressive plan that reduces pain and restores efficient mechanics. The interventions are often exercise-based and hands-on: therapeutic exercise programs, manual therapy such as joint mobilization or soft tissue work, gait retraining, and use of modalities like heat, cold, or electrical stimulation to modulate pain or improve soft-tissue mobility. The aim is functional movement—standing up without assistance, climbing stairs, or returning to sport—achieved through graded challenge and restored biomechanics.
An occupational therapist also assesses movement and strength, but the lens is different. They ask: can this person perform the tasks that define their daily life? OTs evaluate fine motor skills, cognitive processing, visual-perceptual abilities, sensory processing, emotional regulation, and how the environment supports or limits participation. The focus is on activities of daily living (ADLs) and instrumental activities of daily living (IADLs). ADLs include bathing, dressing, toileting, and feeding; IADLs include cooking, shopping, managing money, and work-related tasks. Success is measured in independence, safety, confidence, and the ability to engage in meaningful roles. Interventions blend task-specific training, adaptive strategies, environmental modification, and assistive technology to bridge the gap between ability and participation.
Where physical therapists rebuild the body’s capacity, occupational therapists translate that capacity into everyday life. Consider a person recovering from a knee replacement. A physical therapist will guide progressive strengthening, joint mobility, and ambulation so the knee can support weight and movement. An occupational therapist will focus on getting the person back to routine: stepping into the shower safely, preparing a simple meal while standing, and returning to car transfers. The OT may suggest a raised toilet seat or a long-handled sponge and train the patient in energy conservation strategies to manage fatigue while performing chores. The joint aim is the same—restored independence—but each discipline brings a complementary toolkit.
The methods used by each profession reflect their goals. Physical therapists use graded resistance exercises, neuromuscular re-education, balance training, and manual techniques to correct movement patterns. Their interventions frequently follow measurable progressions: increase hip flexion by X degrees, reduce timed up-and-go by Y seconds, or regain a defined gait symmetry. Occupational therapists use task analysis, modification, and scaffolding to adapt tasks to the person’s abilities. This can include breaking a cooking task into manageable steps, introducing adaptive utensils to compensate for decreased grip strength, or training a worker to use ergonomic adjustments at a workstation. Both disciplines rely on evidence-based practice, but the outcome measures differ. PT outcomes often center on objective physical metrics; OT outcomes center on functional performance and participation in roles that matter to the client.
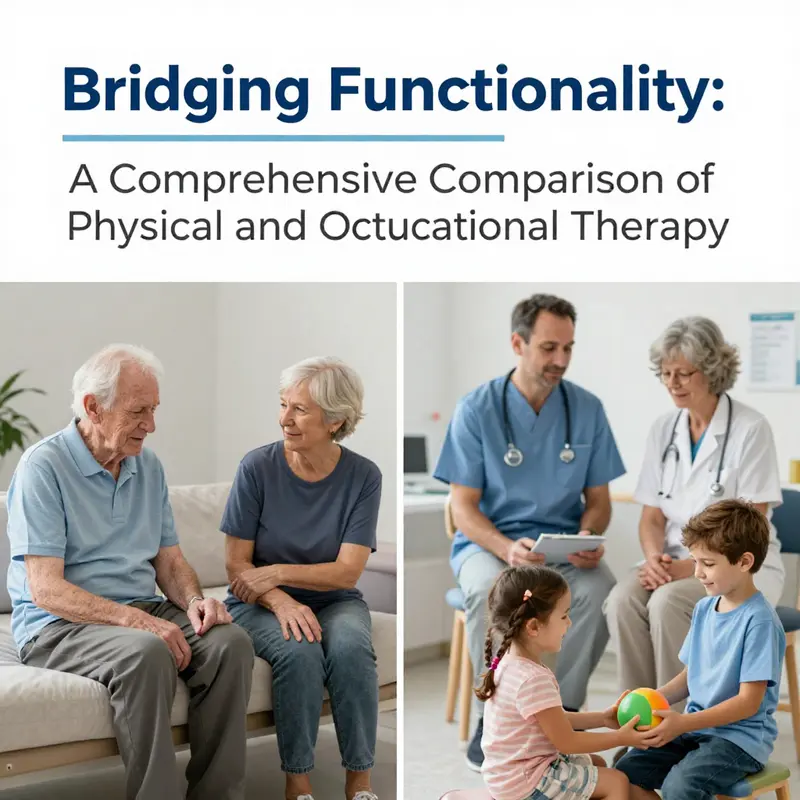
Another important distinction is population and setting. Physical therapists commonly work with people recovering from orthopedic injuries, sports injuries, postoperative rehabilitation, and neurologic conditions that limit mobility. They are central in acute rehab and outpatient clinics focused on movement restoration. Occupational therapists work across a broader functional spectrum that includes children with developmental delays, adults with cognitive or mental health needs, elderly clients with frailty, and people adapting to chronic conditions. OTs frequently work in home health, community settings, schools, and mental health services, addressing not only physical but cognitive and psychosocial barriers to doing what matters.
In neurological rehabilitation, both professions are indispensable. After a stroke, for instance, PTs may emphasize reestablishing safe gait patterns, balance, and lower-limb strength. OTs will concentrate on upper-limb function for self-feeding, toileting, and returning to work-related tasks. The split is pragmatic: walking safely across a hallway may be a PT priority; managing utensils and buttoning a shirt may be an OT priority. When coordinated, these therapies accelerate recovery by addressing both the ability to move and the ability to use that movement in daily life.
Equipment and environmental change also reveal differences. Physical therapy equipment often includes parallel bars for gait training, resistance bands, balance devices, and specialized exercise machines. Occupational therapy equipment includes adaptive utensils, dressing aids, bathing modifications, and task-specific tools. OTs also design environmental modifications like kitchen reorganizing, grab-bar placement, or workstation adjustments. Their work is practical and contextual: a small change at home can be the key to a person remaining independent. For reading about specific OT techniques and tools, see the overview of techniques used in occupational therapy.
Despite these distinctions, the professions overlap and frequently collaborate. Both rely on therapeutic exercise, both use manual techniques, and both value task-specific practice. In rehabilitation teams, the most effective care emerges when PT and OT set shared goals and sequence interventions for cumulative benefit. For example, a person with a spinal cord injury may start with PT-driven mobility and transfers, then transition to OT-led training to perform complex ADLs and employ assistive technology for home and work roles. Collaboration ensures that gains in strength and balance are translated into meaningful, safe activities.
Another key overlap is patient-centered goal setting. Both PTs and OTs work with clients to identify meaningful goals and track progress. This collaborative goal-setting process reduces rehabilitation to more than metrics; it aligns care with the person’s values and life roles. A young parent’s top priority may be safely lifting and carrying a child; an older adult may prioritize returning to gardening. These preferences shape interventions. Therapists tailor plans so improvements in range of motion or grip strength directly support the activities that matter.
Insurance and referral pathways can influence which therapy a person receives first. Acute care often initiates PT to stabilize mobility and safety. If ongoing deficits limit daily tasks, OT is commonly added to address those gaps. In many systems, a physician or other provider refers patients based on assessed needs. Increasingly, interdisciplinary assessment is used so that both PT and OT perspectives inform a unified plan from the start.
Education and training reflect each field’s focus. Physical therapists undergo intensive training in anatomy, biomechanics, exercise prescription, and movement science. Occupational therapists receive in-depth training in activity analysis, assistive technology, cognitive and sensory assessments, and psychosocial aspects of participation. Both professions require clinical internships and continuing education to maintain competency, yet their curricular emphases prepare them for distinct but overlapping roles.
Understanding these differences matters for patients and caregivers. Choosing PT makes sense when the barrier is the capacity to move: pain, weakness, or loss of balance. Choosing OT makes sense when the barrier is the translation of capacity into daily life: safe bathing, workplace demands, or cognitive limitations that prevent task completion. Often, the most efficient pathway is both: rebuild movement and adapt the environment so gains are meaningful immediately.
In practice, success is rarely defined solely by a strength score or the ability to walk a set distance. Success is returning to the morning routine, to work, to hobbies, and to roles that make life meaningful. Physical and occupational therapy each contribute essential pieces to that success. When they work together, rehabilitation becomes not just a series of clinical milestones but a holistic restoration of participation and purpose.
External reference: Cambridge Dictionary’s definition of physical therapy provides a useful, concise description of PT’s emphasis on treatment through physical means: https://dictionary.cambridge.org/dictionary/english/physical-therapy
Internal reference: For a focused comparison of the two fields, see the site covering occupational therapy vs physical therapy.
Techniques, Modalities, and the Harmony of Movement and Daily Living: A Deep Dive into Physical and Occupational Therapy
Physical therapy and occupational therapy share a common aim: to help people recover function and reengage with life after illness, injury, or disability. Yet they approach that goal from different angles. Physical therapy concentrates on restoring movement, strength, balance, and overall physical capacity. Occupational therapy centers on enabling people to perform the activities that give their lives purpose and meaning—daily tasks, work, school, and social participation. Read together, they form a continuum of care that treats the body as a system and the person as a whole, recognizing that movement is the means to living well, while daily activity is the end that keeps life meaningful. In practice, the line between the two professions often blurs, and rehabilitation teams weave their approaches to craft a plan that respects each patient’s unique goals, environments, and hopes for the future. The nuanced choreography between technique and modality in PT and OT highlights not just what each therapy can do, but how they work best when they collaborate in real-world settings.
The core distinction begins with the lens each therapy uses. Physical therapy asks, what must the body be able to do again? It targets locomotion, strength, range of motion, motor control, and pain reduction. A patient recovering from knee replacement, for instance, will walk through a progression of movements to restore gait, rebuild quadriceps strength, and regain the confidence to stand and move independently. This is where the language of PT—exercise therapy, manual therapy, and therapeutic modalities—takes center stage. Exercise therapy is the backbone. It is individualized, progressive, and functional. The program might start with gentle range-of-motion work and gradually incorporate resistance training, balance tasks, and double- or single-leg stance activities. The aim is not simply muscle bulk but the precise neuromuscular control necessary for safe walking, stair climbing, and the subtle transitions that everyday life requires.
Manual therapy and hands-on techniques deepen this restoration. Therapists employ joint mobilization to restore accessory movement and soft-tissue techniques to address stiffness, scar tissue, or localized pain. These approaches are not arbitrary; they are chosen based on the tissue involved and the patient’s response. They complement exercise by reducing pain, improving soft-tissue extensibility, and enabling more effective active movements. When pain limits participation, modalities such as heat or cold, ultrasound, or electrical stimulation can create a window of opportunity—diminishing discomfort, decreasing inflammation, and enhancing tissue healing. In many clinics, these modalities are not standalone treatments but supportive tools that empower patients to perform the exercises that ultimately restore function.
Neurodevelopmental techniques add another dimension in PT, especially for neurological injuries. Bobath concepts, and later proprioceptive neuromuscular facilitation (PNF), emphasize how the brain relearns movement by retraining motor patterns. The work is deliberate and patient-centered: therapists design movement sequences that activate intact neural networks and gradually challenge the patient to refine balance, coordination, and postural control. This approach is particularly vital for stroke survivors or individuals with spinal cord injuries, where the path back to mobility is not simply about strength but about relearning the brain’s commands to move.
On the other side of the rehabilitation table sits occupational therapy, which looks beyond the mechanics of the body to the tasks that matter most in a person’s life. OT asks how the patient engages with daily activities—things as routine as dressing, cooking, bathing, and managing personal care, and as complex as returning to work, driving, or participating in social life. The OT lens is holistic: it recognizes that movement is a means to an end, but the end often involves cognitive, emotional, and environmental factors. The core technique in OT is activity analysis and adaptation. OTs break tasks into components, then reorganize or modify them to fit the individual’s current abilities. A stroke survivor might relearn the steps of making a meal by simplifying the sequence, using one-handed techniques, and introducing adaptive equipment. A person with arthritis might switch to ergonomic tools in the kitchen, or install supports that reduce strain during grooming and dressing. The emphasis is not merely on execution but on independence and safety within daily routines.
Fine motor and sensory integration training is another hallmark of OT. Dexterity, hand-eye coordination, and tactile processing are refined through purposeful activities that resemble real-life tasks. For children with developmental delays, OT can nurture hand skills that underpin writing, self-feeding, and play. For adults recovering from brain injury, it can translate into practical skills like managing buttons and zippers, organizing a work desk, or coordinating fine motor tasks needed for vocational tasks. Cognitive rehabilitation is equally central. Attention, memory, problem-solving, and executive function are often disrupted after brain injuries or strokes. OTs tailor activities that challenge the mind while staying grounded in meaningful tasks—planning a route to a grocery store, sequencing steps for a morning routine, or organizing medications. Such work helps rebuild autonomy not only by enhancing physical capability but by restoring cognitive strategies that support daily living.
Environmental modification and adaptive equipment are the practical theater where OT and PT converge but apply different logic. PT often considers how movement occurs in a clinical space or a rehabilitation setting, focusing on gait, transfer, and balance strategies that translate to safer ambulation at home. OT, however, frequently takes the broader view of a patient’s living and working environments. A home safety assessment might reveal the need for grab bars, improved lighting, or rearranged furniture to reduce the risk of falls. An office or a classroom can be optimized through layout adjustments, assistive devices, and workflow adaptations that empower the person to participate with dignity and competence. The environmental dimension is where OT shines in reducing barriers to independence, whether at home, in school, or at work.
The two disciplines rarely operate in silos. In neurorehabilitation centers, orthopedic clinics, and long-term care facilities, PTs and OTs collaborate as a coordinated team. Each professional brings a complementary perspective that respects the patient’s goals and the realities of the environment in which care unfolds. Consider a patient recovering from a brain injury who aims to return to work. PT will address locomotion and strength, ensuring safe mobility through the workplace and the physical demands of the job. OT will then partner to translate that mobility into functional work tasks—typing, driving, carrying objects, or managing a workstation. The result is not merely a restored gait or better balance; it is a restored capacity to perform the tasks that confer employment, purpose, and identity.
This collaborative model is supported by a growing body of evidence that emphasizes patient-centered outcomes. The most compelling data show that when PT and OT are coordinated, patients experience more rapid improvements in both mobility and daily functioning. They walk sooner, perform self-care with greater independence, and resume valued activities with fewer safety concerns. The patient’s narrative matters most: the story of regaining the ability to dress, prepare meals, or return to a favorite hobby is as important as the measurable gains in range of motion or muscle strength. A rigorous rehabilitation plan recognizes that progress in movement can unlock a broader spectrum of participation, while gains in daily activity can reinforce motivation to continue therapy.
The interdependence of techniques and modalities in PT and OT is also a reminder of the human element in rehabilitation. Therapists tailor their interventions to the person who sits before them—their age, culture, goals, and daily rhythms. A knee-replacement patient may be coached through a progressive activity ladder that culminates in a walk to the mailbox and a climb of a few stairs without a cane. A stroke survivor might practice cooking a simple breakfast to rebuild sequencing, planning, and confidence, while also addressing the household’s safety concerns. In pediatric settings, OT can support school readiness and social participation, while PT helps with gross motor milestones that pave the way for broader engagement with peers and activities. Across ages and diagnoses, the underlying philosophy remains constant: interventions should empower individuals to participate in the life they want, in the places where they live, work, play, and learn.
The modalities themselves—whether movement-based, hands-on, or environmental—are not ends in themselves. They are instruments that enable people to meet meaningful goals. The choices clinicians make are guided by evidence, patient preferences, and the realities of everyday life. Therapeutic exercises are not an abstract ritual; they are the scaffolds that build strength, stamina, and control. Manual therapy is not a cosmetic touch; it can unlock the ability to reach, grip, or stabilize a joint. Sensory integration, cognitive rehab, and psychosocial strategies belong in the repertoire because rehabilitation is as much about feeling capable and connected as it is about being independent. And when a patient’s home or workplace is in view from the start, therapy plans stay grounded in what will be possible once discharge occurs.
In this sense, the most powerful narrative about physical and occupational therapy is not one of rivalry but of partnership. The patient journeys through a landscape where movement and daily life are not separate goals but intersecting pathways. PT and OT meet the person where they are, respect the pace of recovery, and stretch toward a future where mobility supports meaningful participation. The path is rarely linear; it bends with pain, fatigue, and evolving goals. Still, the guiding compass remains clear: restore body function, enable daily competence, and nurture the confidence required to rejoin the people and activities that matter most. The result is a rehabilitative experience that honors both the body and the life it supports.
For readers curious about how these two professions compare in practice, a concise synthesis often emerges: physical therapy returns the body to motion, while occupational therapy teaches the person to live within that motion with independence and safety. This complementary dynamic matters not only in hospitals but in homes, schools, workplaces, and communities. It invites a holistic view of healing that transcends the clinic walls and recognizes that the ultimate objective is quality of life—dignified, engaging, and sustainable. If you want to explore this distinction more explicitly in the context of everyday considerations, see the discussion on occupational therapy and physical therapy differences in the linked resource that compares their roles directly: occupational-therapy-vs-physical-therapy.
As this chapter illuminates, the modalities and techniques of PT and OT are best understood as a shared toolkit. The real artistry lies in how clinicians blend them to honor each patient’s priorities. In a world where return to meaningful activity is the horizon, movement and daily life are not two destinations but a single, evolving journey. The synergy between physical and occupational therapy shapes this journey, offering a comprehensive path from impairment toward participation—the goal that sits at the heart of rehabilitation itself.
External resource: https://www.apta.org/what-is-pt
null
null
Walking the Line Between Movement and Meaning: Outcomes, Synergy, and the Real-World Reach of Physical vs Occupational Therapy
In rehabilitation, progress is often described as a journey rather than a single destination, and the way that journey unfolds depends on the lens you bring to it. Physical therapy and occupational therapy share a common goal: to help people live fuller, safer, more independent lives. Yet they chart different maps across the terrain of function. Physical therapy centers on movement itself—how people walk, stand, bend, and balance. Occupational therapy centers on meaningful human activity—dressing for the day, preparing a meal, returning to work, managing a household, or engaging with loved ones. That core distinction matters because it shapes both the expectations of recovery and the way success is measured over time. When clinicians align these two disciplines, the resulting rehabilitation plan becomes more than a sum of parts; it becomes a coordinated conversation about how best to restore not only physical capability but also daily meaning and social participation. The longitudinal question is not only, Can a patient walk again? but also, Can a patient perform the tasks that give life structure and dignity, even when some movement remains limited? In chronic conditions where trajectories are unpredictable, such as multiple sclerosis, this integrated perspective becomes all the more essential, offering a framework to tailor interventions toward both mobility and the daily activities that confer autonomy and purpose.
From the standpoint of outcomes, physical therapy tends to foreground objective, movement-centered metrics. Clinicians track gait speed, balance scores, endurance, and spasticity, translating improvements into clearer steps—literally—toward safer ambulation and more efficient movement. The 6-Minute Walk Test, for instance, remains a common yardstick for endurance, while balance scales gauge whether someone can navigate a room without the fear of a fall. In neurologic conditions, strengthening programs and motor retraining are designed to restore patterned movement that may have weakened or become inefficient due to injury, surgery, or disease. In this sense, PT acts as a regimen for the body’s infrastructure: the bones, joints, muscles, and neural pathways that underpin ability. Effectiveness, measured through these objective metrics, directly impacts a patient’s ability to perform basic physical tasks with less effort and pain, to conserve energy for the moments that matter most, and to maintain independence in daily life tasks that require mobility as a foundation.
Occupational therapy, by contrast, widens the lens toward the person in his or her environment. OT’s strength lies in translating physical capability into real-world function. It asks: How does a condition alter a person’s capacity to carry out ADLs—dressing, bathing, cooking, managing personal care? How does it affect IADLs—driving, shopping, managing finances, communicating with colleagues? OT practitioners examine not only physical constraints but cognitive, emotional, and environmental factors that shape performance. They examine fatigue, attention, memory, and executive function within the context of daily routines. They also consider the surroundings in which those routines unfold—home layouts, workplace demands, community access, and social supports. The aim is to bridge the gap between what a patient can do in a clinic and what a patient needs to do to participate meaningfully in life, with adaptations that can include environmental modifications, assistive devices, or new strategies for energy management. In MS, for example, OT often targets fatigue management, task simplification, and safety in the home or workplace, helping patients reconfigure their environments to align with fluctuating capacities. The outcome here is not only whether an activity is completed but whether it can be integrated into a person’s day with a sense of control, ease, and satisfaction.
A deeper look at how these outcomes are captured reveals not just different measures but different philosophies of success. PT outcomes emphasize physical capacity and functional independence through movement. The improvements are tangible in the body: stronger muscles, better posture, steadier gait, reduced spasticity, and longer endurance. These gains frequently translate into reduced reliance on assistive devices and fewer activities limited by pain or fear of instability. But the durable effect of PT is not measured only in miles walked or seconds shaved from a timed task; it is reflected in a patient’s confidence to move through daily life with less cognitive load and less energy expenditure, enabling more room for participation in family life, community activities, and self-identified goals.
OT outcomes, meanwhile, center on participation and satisfaction. A common framework is patient-reported outcomes that capture perceived ability to perform daily tasks, quality of life, and satisfaction with life roles. The Canadian Occupational Performance Measure (COPM) and similar tools foreground the patient’s own priorities, identifying activities that matter most and tracking changes in how difficult those activities feel. The success of OT often appears as a patient’s return to valued routines—safe cooking for a caregiver, managing medications without confusion, or driving when possible—enhanced by adaptive strategies, environmental tweaks, and the deliberate pacing of tasks to counter fatigue and cognitive load. In this sense, OT approaches rehabilitation with a human-centered compass: not merely how well a person can move, but how well a person can live with the realities of their condition, maintain a sense of autonomy, and sustain meaningful roles in family, work, and community. The emotional and psychological dimensions of recovery are not afterthoughts; they are integral to the sense that life remains worth living, even when full restoration of function is not possible. This emphasis on meaning, purpose, and adaptation often correlates with improvements in mood, motivation, and resilience, which in turn can positively influence engagement with physical tasks as well.
The most compelling argument for a coordinated PT–OT approach is the synergy that emerges when movement and meaning are developed in tandem. In rehabilitation, movement precision created by PT can liberate individuals to participate more fully in tasks that OT targets, while OT’s emphasis on daily life can ground PT exercises in real-world relevance. When therapists collaborate, they can sequence interventions to maximize both physical gains and practical competence. For example, a patient recovering from a brain injury might work with PT on gait and balance to reduce fall risk while simultaneously engaging with OT to relearn how to manage a kitchen or navigate a workplace task with appropriate adaptations. The patient benefits from a more coherent narrative of recovery, where improvements in strength, endurance, and balance are immediately connected to tangible improvements in daily living and social participation. The result is a rehabilitation plan that does more than restore a body part or a skill; it sustains and enhances the person’s overall quality of life.
Measuring the impact of such an integrated approach requires attention to both categories of outcomes and to how they interlock over time. Objective gait improvements can provide a platform for patients to attempt more complex tasks, which OT can then adapt to the patient’s home or work environment. Conversely, improvements in the ability to perform daily tasks in a controlled setting may reveal new goals for movement training in PT, such as hiking, dancing, or negotiating stairs with improved confidence. The literature increasingly supports this integrated model, noting that comprehensive rehabilitation that combines PT and OT tends to yield better functional status and more robust social participation than isolated therapy alone. Yet the field also recognizes that outcomes must reflect the lived reality of patients with chronic and fluctuating conditions. The “outcomes movement” in healthcare, as scholars frame it, pushes clinicians to capture a broader spectrum of benefits: functional status, social integration, emotional health, and the ability to return to meaningful work or community life. It is not enough to know that a patient can walk farther if that person cannot return to caregiving, volunteering, or part-time employment that sustains identity and purpose.
The patient journey in MS provides a vivid illustration of how PT and OT work together. MS can present with variable symptoms, including impaired mobility, fatigue, cognitive changes, and sensory or visual challenges. A PT plan might prioritize gait training, fall prevention, and muscle strengthening to stabilize movement and reduce fatigue associated with poor posture and inefficient walking. A therapist will monitor fatigue levels and adapt intensity to avoid overexertion, a common barrier to progress in chronic neurological conditions. The OT plan would simultaneously address fatigue management, task simplification, and home safety, ensuring that when mobility improves, the person can still perform essential tasks and adapt to the environment without constant fatigue or risk. The combination of these strategies—improved walking capacity paired with smarter energy use and safer, more accessible living spaces—creates a more resilient daily life. The value lies not just in enabling a patient to move but in supporting the patient to participate in work, family life, and chosen activities with a consistent sense of control and competence. This resonates with patients who describe their rehabilitation as a chance to re-engage with life, rather than a narrow pursuit of physical restoration.
For clinicians seeking to optimize outcomes, the evidence increasingly favors integrated, goal-oriented rehabilitation that respects patient priorities. This means engaging patients early in goal setting, aligning PT and OT plans with what matters most to the patient, and maintaining flexibility to accommodate fluctuating symptoms. It also means recognizing the emotional and psychological dimensions of recovery and incorporating strategies that support mood, motivation, and self-efficacy. The practical implication is a care pathway that moves beyond siloed sessions toward a cohesive program in which therapists communicate, co-treat, and co-monitor progress. When done well, patients experience not only measurable improvements in performance metrics but also a sustained sense of autonomy and purpose that persists across the daily routines that define a life well lived.
One of the subtler yet crucial benefits of this integrated approach is its adaptability to different populations and settings. In aging populations, OT’s environmental modifications and energy conservation strategies can reduce the stigma and effort associated with disability, allowing older adults to maintain independence in home and community. In pediatric populations, OT may focus on play-based activities that promote skill development while PT can address gross motor milestones and muscular development, ensuring that children grow up with both the mobility and the capacity to participate in school and social life. In adult rehabilitation after injury or surgery, a combined PT–OT plan helps individuals regain work readiness while preserving safety and functional autonomy in daily living. Across these contexts, the aim remains constant: to empower individuals with the physical capacity to move and the practical means to use that capacity in ways that matter most to them. In doing so, rehabilitation becomes less about matching a predefined template of recovery and more about sculpting a personalized path that aligns movement with meaning, pace with purpose, and body with life.
To readers navigating these choices for themselves or loved ones, a practical takeaway is to seek a care team that emphasizes collaboration and patient-centered goals. Ask about how the team plans to measure progress, how goals are selected, and how the two disciplines will coordinate to ensure that improvements in movement translate into tangible gains in daily life. Consider also the broader social and environmental supports that influence outcomes: home modifications, transportation, caregiver training, and access to community resources all shape the likelihood that gains in the clinic will translate into lasting, meaningful participation. The best rehabilitation experiences treat PT and OT not as competing domains but as complementary pathways that, when aligned, unlock a fuller range of human function and a richer sense of personal agency. That synergy matters because it speaks to the heart of rehabilitation: not merely returning to baseline but creating a life that feels navigable, hopeful, and worth pursuing every day.
For readers curious about distinctions that can guide initial decisions or educational exploration, there is value in understanding the nuance between movement and meaning. A concise way to frame it is to view physical therapy as the engineer of locomotion and strength, and occupational therapy as the architect of daily life design. Each discipline offers unique tools, but their impact magnifies when they work as a single strategy aimed at the patient’s lived experience. The knowledge that outcomes extend beyond scores on a test to the quality of daily life can help clinicians, patients, and families align expectations and celebrate progress in a more holistic way. As research continues to illuminate the benefits of integrated rehabilitation, the practical reality remains clear: the most effective recovery journeys honor both movement and meaning, and they cultivate a sense of control that persists long after the last therapy session.
For further reading that situates these ideas within current rehabilitation science, explore the broader literature on outcomes in MS and related conditions, which highlights how comprehensive approaches can support long-term independence and quality of life. What is the difference between physical therapy and occupational therapy? The overarching takeaway is simple yet profound: when PT and OT work together, patients are more likely to reclaim both the steps they take and the steps they wish to take in life. External readers seeking a deeper evidence base can review the latest synthesis in rehabilitation science, such as the National Library of Medicine’s discussion of outcomes in multiple sclerosis rehabilitation, which underscores the value of integrating physical and functional goals over time. For a comprehensive review, see the external resource: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8504321/
Final thoughts
In summary, physical therapy and occupational therapy each have their unique strengths and specialized approaches to patient care. For business owners in healthcare, understanding these differences is crucial in ensuring complementary services that address both physical rehabilitation and functional independence. Whether through focused physical therapy practices or comprehensive occupational therapy strategies, offering a diverse range of therapeutic services can significantly enhance patient care outcomes and satisfaction.