In today’s society, helpers in various professional capacities play an indispensable role in enhancing the quality of life for individuals and communities. From healthcare to fitness and emergency services, these careers are dedicated to providing essential support and fostering well-being. In this exploration, we will delve into five vital professions: home health aides, personal trainers, paramedics, rehabilitation specialists, and 911 dispatchers. Each chapter will shed light on their unique contributions, emphasizing the growing demand for skilled helpers and their impact on society at large.
The Quiet Frontline: How Home Health Aides Shape Lives and Careers in a Changing Health System
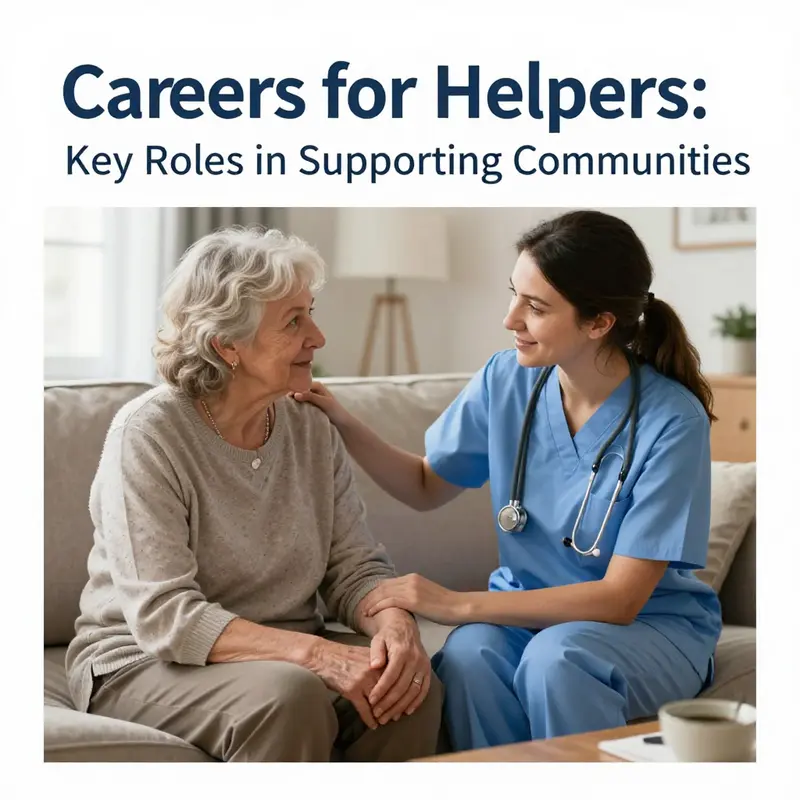
Across the health system, many of the most meaningful acts occur in the rhythm of daily life. Home health aides stand on a quiet frontline, moving through living rooms and kitchens to translate clinical plans into practical, compassionate care. They do more than complete tasks; they preserve dignity, sustain independence, and nurture human connection. For many clients, the ability to stay in their own homes hinges on the consistent presence of a caregiver who can balance routine support with sincere companionship. The alternative—an institution that feels distant and unfamiliar—can carry emotional costs that ripple through families and communities. In home-based care, comfort and safety are not secondary goals; they are the core of a philosophy that sees the person first, the illness second, and the environment as a critical ally in healing and daily living. When a client remains at home, the benefits extend beyond the individual. Families find relief, and the healthcare system gains efficiency through reduced hospital visits and smoother care transitions. This is not a dramatic sprint but a steady, enduring commitment that makes tangible differences in people’s lives and in the stability of whole neighborhoods.
The work of home health aides centers on practical, everyday support that helps people manage the realities of illness, aging, or disability. A typical day might begin with helping a client bathe and dress, preparing meals that meet dietary needs, and arranging medications along with reminders to take them on time. Light housekeeping and safety checks follow, ensuring clear paths through clutter and potential hazards. Yet behind these routines lies a deeper skill: the ability to listen well, to observe subtle changes in mood, appetite, energy, or mobility, and to report concerns promptly to nurses or supervising clinicians. Observational acuity is as essential as any manual task, because small changes can signal a larger shift in health. In other words, the job blends practical technique with attentive presence, a combination that supports both physical health and emotional well-being.
The value of this role grows as the population ages and preferences shift toward home-based care. Home health aides provide a bridge between clinical teams and everyday life, translating medical instructions into feasible routines that respect a client’s routines, culture, and tastes. Their presence can reduce the need for more costly or disruptive forms of care, while enabling family members to participate in meaningful ways without bearing the full burden of daily supervision. The benefits, however, extend beyond cost and convenience. The companionship offered in moments of isolation can lift spirits, reduce anxiety, and reinforce a sense of autonomy. This is care that honors not only illness or impairment but the broader arc of a person’s life, relationships, and sense of self.
To succeed in this field, prospective aides enroll in formal training programs that cover infection control, basic anatomy, safety protocols, and patient rights. Those courses lay a sturdy foundation, but the strongest practitioners also cultivate soft skills that technology cannot replace. Empathy guides every interaction, turning routine tasks into acts of reassurance. Active listening builds trust with clients and their families, who often seek a caregiver’s steady, nonjudgmental support. Reliability is proven in the quiet cadence of a schedule kept with punctuality and consistency. Cultural sensitivity matters as well, because care happens within a family’s belief systems, values, and daily rhythms. The best aides balance technical knowledge with genuine human warmth, creating a caregiving environment where clients feel seen, respected, and safe.
Career progression in this field is real and reachable. Many aides advance to become certified nursing assistants, a step that often opens doors to broader clinical responsibilities and more formal recognition. Some move into supervisory roles within home health teams, coordinating care plans, mentoring new staff, and ensuring that standards of practice are consistently met. Each of these transitions rests on ongoing learning: additional certifications, specialized trainings, and reliably applying lessons from real-world experience. Even with these pathways, the essence of the work remains constant—sustaining independence, dignity, and comfort for people who rely on home-based care. In this sense, a career as a home health aide is not a temporary job harvested for a paycheck; it is a vocation that deepens with time, skill, and a growing sense of purpose.
The demand for in-home care continues to rise, driven by demographic shifts and preferences for aging in place. Communities are watching a widening gap between the needs of aging residents and the availability of robust in-home support. This gap creates meaningful opportunities for those who want to contribute to health and well-being in a way that respects autonomy and personal history. It also invites a broader conversation about how care is organized and funded, and how frontline workers are supported so that their work remains sustainable and fulfilling. In this evolving landscape, home health aides are not only caregivers; they are partners in a collaborative system that seeks to keep people connected to their homes, families, and routines while receiving the care they need.
The work environment itself offers a unique blend of independence and teamwork. Aides often manage their own caseloads, setting priorities within safety guidelines and care plans. This autonomy is balanced by regular communication with nurses, therapists, and social workers who contribute clinical insight and monitor progress. The relational aspect of the job is at once demanding and rewarding. A brief moment of shared laughter, a steady voice during a anxious afternoon, or a practical demonstration that restores a client’s sense of control can be the most meaningful outcomes of a day. For families, the presence of a reliable aide can transform a home from a place of worry into a space where daily life continues with as much normalcy as possible. Such outcomes are not measured only in task completion but in the intangible sense that life continues with dignity and hope.
The profession does face challenges. The emotional labor of constant care, the physical demands of assisting mobility, and the realities of demanding schedules require resilience and strong support networks. Compensation and recognition have historically varied by region and employer, creating disparities that new policies and workforce development efforts strive to address. Yet, even amid challenges, the social significance of home health aides remains clear. They enable care that is person-centered, flexible, and deeply attuned to each client’s history and preferences. They offer continuity in moments that can otherwise feel fragmented, and they sustain families by sharing responsibility and expertise. The sense that one’s daily work matters—truly matters—helps explain why many aides stay in the field for years, developing expertise, forming trusted relationships, and finding opportunities to mentor others.
Looking ahead, technology will increasingly interact with hands-on caregiving in ways that enhance safety and efficiency without erasing the human touch. Digital scheduling, remote monitoring, and data-driven insights can help families and clinicians coordinate care more precisely. Yet technology cannot replace the heart of the job: the ability to listen, to adapt, and to respond with compassion in real time. The strongest practitioners blend practical know-how with emotional intelligence, creating an atmosphere of partnership with clients and families. In the broader arc of careers for helpers, home health care provides a compelling model: it demonstrates how technical competence and human connection can fuse into a meaningful, sustainable profession. It shows that care work is not a fallback option but a deliberate, principled career path that continually earns trust, expands capacity, and renews communities.
For readers exploring the wider landscape of helping professions, a broader map exists that highlights many pathways beyond direct care. A resource like the post on seventeen careers for helping people offers a useful overview of how compassionate work can unfold across settings, from clinical environments to community-based roles, and how skill sets can transfer between situations. For a concise synthesis of related roles and opportunities, see this overview: seventeen careers for helping people.
As this chapter ties back to the overarching topic, it becomes evident that a career as a home health aide is more than a job description. It is a sustained commitment to support the well-being of others in a way that honors their autonomy and dignity. It embodies the idea that helpers—from aides to nurses to therapists—are essential gears in a large, interconnected system. Each role contributes to a society that values care as a practice, not merely a phrase. The work invites ongoing learning, opportunities for advancement, and, above all, the chance to touch lives in tangible, enduring ways. In the tapestry of careers for helpers, home health aides offer a crucial thread—one that binds compassion to competence, and personal purpose to public health.
For a broader reference on responsibilities and outlook for frontline care work, see the U.S. Bureau of Labor Statistics overview of home health aides: https://www.bls.gov/ooh/healthcare/home-health-aides.htm
null

null
Paramedics on the Frontline: Lifesaving Careers for Helpers in Emergency Medical Services
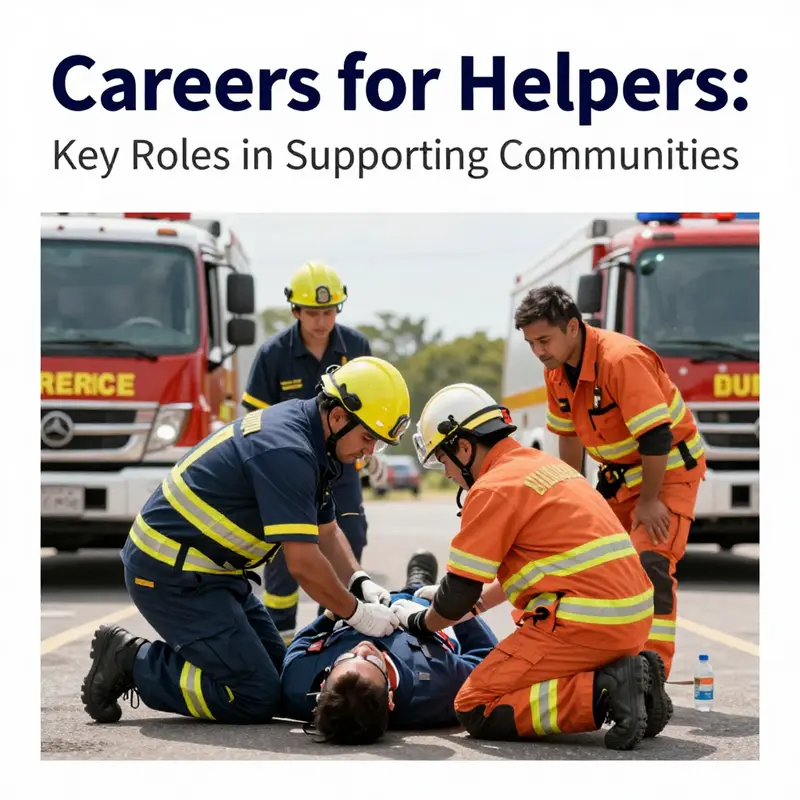
Paramedics occupy a distinct place in the ecosystem of helping professions. They are summoned to scenes that demand calm, quick thinking, and technical prowess, yet they also carry the heavy responsibility of guiding frightened, vulnerable people through moments that can define outcomes. In the broad narrative of careers for helpers, paramedics stand as a bridge between immediate bedside care and the broader arc of the medical system. They arrive where danger has disrupted routine life, and they stay long enough to stabilize, resuscitate, and secure a path toward recovery. This calling blends science with service, urgency with empathy, and the grit of the streets with the precision of clinical practice. In a sense, paramedics personify the core idea that helping identities are built not merely on intent but on the capacity to act decisively when time compresses into a singular, life-altering moment.
The heart of a paramedic’s work lies in rapid assessment and immediate treatment. On arrival, the priority is to assess the patient’s condition with calm thoroughness even as surrounding chaos unfolds. Paramedics must be fluent in identifying life-threatening signs and acting on them without hesitation. This includes performing cardiopulmonary resuscitation when needed, managing airways to ensure breathing, controlling bleeding, and recognizing shock. These are not rote tasks but dynamic judgments that shift with every new piece of information gathered from the scene, the patient, or the responders already on site. The ability to read a body under pressure—gauging whether a patient is deteriorating or stabilizing—depends as much on experience and instinct as on protocol. Skills are exercised at the edge of what can be safely done in the moment, and the consequences of decisions can be measured in minutes, not days.
Beyond the basics, paramedics carry out advanced medical procedures that set them apart from many other emergency responders. They are authorized to administer medications, interpret electrocardiograms, use defibrillators, and perform airway management techniques such as intubation when necessary. In more complex scenarios, they may perform procedures like needle decompressions in cases of certain types of chest injuries. These capabilities transform the ambulance into a mobile clinical unit focused on stabilizing patients for the trip to a hospital. The transport phase is not a simple conveyance; it is a continuation of care. Paramedics monitor vital signs, adjust treatments as the patient’s condition evolves, and communicate critical information to hospital teams so that the receiving facility is prepared for what comes next. The seamless relay of information and the sustained attention to the patient during transit are as essential as the initial scene management itself.
The education and training path to become a paramedic reflects a rigorous commitment to mastery. Most programs run from twelve to twenty-four months and immerse students in anatomy, physiology, pharmacology, trauma care, and emergency medicine. Hands-on clinical experience is a cornerstone of this education, with hundreds of hours spent in real-world settings, often including ride-alongs with seasoned paramedics. Certification, such as the national registry exams and state licensure, marks the formal entry into the profession, but learning does not end with the diploma. Paramedics continually refine their practice through ongoing in-service training, simulations, and case reviews that illuminate both successes and missteps. The arc from student to practicing paramedic is characterized by a gradual expansion of responsibility and a deepening understanding of when to act, when to escalate, and how to coordinate with other professionals under pressure.
Demand for paramedics has grown as populations shift and health systems adapt to new challenges. In the United States, employment projections indicate growth that outpaces many other fields, driven by population density and the expanding role of EMS in community health strategies. The U.S. Bureau of Labor Statistics highlights a faster-than-average outlook for paramedics over the coming decade, underscoring how essential these roles are to public safety and health access. Across the Atlantic, the scope of practice is evolving in places like the United Kingdom, where paramedics have gained expanded prescribing rights, enabling them to administer a wider array of medications independently. These shifts reflect a broader theme within the helping professions: the necessity for highly trained responders who can make timely decisions in time-sensitive environments while aligning with evolving standards of care. The result is a career path that is both practically demanding and deeply consequential for patients and communities.
Working as a paramedic presents a compelling blend of intensity and purpose, yet it is not without significant challenges. The work environment routinely places professionals in high-stress situations, from motor vehicle crashes to heart attacks, from industrial accidents to natural disasters. The physical demands are substantial: lifting, carrying, and maneuvering patients and gear in confined spaces or unstable terrains. The emotional toll is equally real, as paramedics witness trauma, loss, and sometimes long recoveries. The exposure to life-and-death scenarios can lead to mental health strain, prompting EMS organizations to invest in peer support programs, debriefings, and ongoing mental health resources. Individuals who thrive in this field tend to bring resilience, clear communication, and a temperament that stays focused amid uncertainty. They also cultivate a strong sense of duty: a belief that the person in the back of the ambulance deserves both competent medical care and compassionate humanity at the most vulnerable moments of their lives.
Within this framework of service, paramedics increasingly act as connectors within the broader health system. Their on-scene assessments guide not only immediate care but decisions about the most appropriate destination for patients. They communicate with hospitals to prepare for arrivals, ensuring a smoother handoff that can reduce delays and improve outcomes. This aspect of their role—operational coordination—illustrates how modern emergency medicine depends on a team-oriented approach that spans prehospital care and hospital-based treatment. Paramedics thus embody a professional identity that intertwines clinical expertise with collaborative practice. They are not merely responders but integrators who bring together the knowledge, equipment, and support networks that patients rely on in moments of crisis.
As technology reshapes many fields, paramedics are embracing innovations that enhance both speed and accuracy. AI-assisted triage tools are becoming more common in the field, helping responders prioritize interventions when time is scarce. Digital patient records carried by paramedics streamline information transfer to hospitals, enabling clinicians to pick up where the field left off with a clearer understanding of the patient’s recent history and current needs. Yet technology serves the human element rather than replacing it. The art of bedside care remains anchored in listening to patients, validating their fears, and explaining what is happening in language that is accessible and reassuring. The human touch—empathy delivered in the back of a loud, moving vehicle—continues to distinguish the paramedic’s work and to sustain the trust that patients and families place in responders.
Looking ahead, the field invites specialization and expanded roles that keep pace with community health priorities. Some paramedics pursue critical care transport, bringing high-level care to patients who require complex management during the transfer between facilities. Others engage in tactical medicine, disaster response, or public health initiatives that extend the reach of EMS beyond single-incident responses. The profession is also recognizing the importance of supporting the mental health and well-being of its practitioners through structured peer support and accessible counseling resources. As EMS systems evolve to address broader social determinants of health, paramedics may increasingly collaborate with social workers, community health workers, and other professionals to connect patients with the resources they need, from housing to follow-up care. The career, thus, is not only about the immediacy of a single rescue but about contributing to a continuum of care that can alter life trajectories for individuals and families.
For readers who are exploring the wider landscape of helping careers, the paramedic pathway offers a vivid example of how specialized skill, rapid decision-making, and compassionate communication converge to create meaningful, lifelong work. It invites consideration of one’s tolerance for high-stakes environments, willingness to engage in continuous learning, and commitment to serving communities in moments when options feel limited. If you are drawn to the idea of a career that blends science, action, and service, this field presents a clear and compelling route. And for those who want to survey the broader spectrum of helping professions, a concise overview can be found in resources that map the many paths available to people who want to make a tangible difference in others’ lives. For a broader view on the array of helping careers, consider a quick overview in 17 Careers for Helping People, which can offer perspective on where paramedics fit within the larger ecosystem of allied and frontline professions. 17 Careers for Helping People.
The paramedic story is a reminder that careers for helpers are not one-size-fits-all. They require discipline, continuous learning, and a steady commitment to serving others under pressure. They demand the courage to face situations that most people would rather avoid, and they reward this courage with tangible benefits—the chance to save lives, to reduce suffering, and to guide people toward a path of stability after moments of crisis. In this light, paramedics are more than responders; they are anchors in communities, ready to lift people up when they need it most. They embody the best of what helping professions strive to be: practical, principled, and profoundly human.
External resource: For a comprehensive overview of the role, duties, salary expectations, and licensing considerations for paramedics, see the U.S. Bureau of Labor Statistics resource What Does a Paramedic Do? (And How to Become One). https://www.bls.gov/careerinfo/
null
null
Listening Under Pressure: How 911 Dispatchers Orchestrate Lifesaving Help and Shape Careers in the Helper World
In the chain of care that modern societies rely on, the voice that begins every emergency response is not the siren or the stretcher, but the calm, deliberate cadence of a 911 dispatcher. They stand at the juncture where confusion meets possibility, where a call can pivot from fear to action in a heartbeat. Their work is not a single skill but a composite art: the ability to listen with clarity, to translate chaos into concrete needs, and to marshal the right teams at the exact moment they are most needed. To call these professionals merely operators would miss the essence of what they do. They are lifelines, architect of timing, and the human anchor that steadies a crisis long enough for responders to arrive with the right tools and the right plan. In this way, dispatchers embody the heart of the broader field explored in this article on careers for helpers: a vocation where listening, coordination, and responsible action create pathways for help to travel from a single voice to a coordinated response that saves lives and sustains communities.
The daily responsibilities of 911 dispatchers revolve around three core actions that, taken together, determine the effectiveness of the entire emergency response system. First, they gather information. The caller’s story is the raw material from which all subsequent decisions flow. The dispatcher must quickly sift facts from noise, identify the nature of the emergency, and distinguish between priorities that require police, fire, or medical teams. This is not an exercise in verbosity; it is a short, precise exchange in which every question has a purpose, every pause carries meaning, and every bit of detail—locations, hazards, injuries, additional witnesses—can dramatically alter the course of events. Second, dispatchers assess the situation. They calibrate urgency, triangulate risk, and anticipate what the responders will encounter on the ground. This assessment must be fast, but not reckless, and it must stay adaptable as new information arrives. A momentary misjudgment about a scene’s danger can cost precious minutes or compound a crisis, so the ability to stay level, to hold competing possibilities in balance, and to adjust the plan as conditions change is a defining trait of expertise in this field. Third, dispatchers dispatch services. They translate assessment into action by alerting the appropriate responders, relaying critical details, and providing updates as the situation unfolds. The dispatch center becomes a command post that doesn’t merely relay instructions but coordinates a live operation across multiple agencies. In essence, the dispatcher’s work is the invisible scaffolding of emergency response—the structure that holds together time, information, and personnel so that help arrives where it is needed, when it is needed, with the clarity needed to act.
What makes this work deeply human is not only the accuracy of information but the temperament that accompanies it. A dispatcher’s voice carries weight, but it must also convey empathy. The caller may be frightened, disoriented, or overwhelmed by trauma. The ability to listen with patience, to acknowledge distress without becoming overwhelmed by it, and to guide the caller toward making clear, actionable statements is a subtle duet. It requires more than procedural familiarity; it requires emotional intelligence in the service of public safety. The words a dispatcher chooses—and the way those words are delivered—can either anchor a terrified person to a safe course of action or contribute to confusion in the critical moments before responders arrive. This synergy between technical skill and human sensitivity is at the core of why dispatchers are essential helpers in the community. They are not simply the first link in a response chain; they are active partners in every rescue, every careful medical handoff, every evidence-based decision that shapes an investigation and the eventual recovery of a person in need.
Yet even the most capable professionals operate within the bounds of knowledge and training that govern this field. A 2025 study highlighted a significant gap in the knowledge base of many dispatchers: while they recognize their role as information gatherers and coordinators, many lack a robust understanding of how subtle language cues can distort eyewitness memory. Lead questions, post-event details, even the cadence of a question can influence what a caller remembers and how accurately those memories can later be used in investigations or court proceedings. This insight is not about blame but about quality improvement. It exposes a vulnerability in the information chain that, if left unaddressed, can undermine the reliability of evidence and, by extension, the integrity of subsequent decisions. The study’s framing is practical: it identifies a concrete area where the field can raise its baseline through targeted education and practice so that every dispatch conversation preserves as much accuracy as possible, even under pressure.
The implications of this gap extend beyond the discipline of dispatch work and into the broader ecosystem of care and justice. Training that foregrounds cognitive psychology—how memory works, how questions can unintentionally steer recall, and how to ask neutrally—can transform a dispatcher’s practice. Standardized protocols for information collection provide a guardrail against variation that might otherwise creep in under stress. Rather than relying on improvisation in moments of upheaval, dispatch centers can implement consistent methods that help ensure every piece of information is captured with fidelity. The recommended approach is ongoing professional development: regular, scenario-based training that keeps knowledge fresh and aligned with current research, and that invites dispatchers to reflect on their communication habits in light of new findings. In a field where milliseconds matter, such ongoing learning is not a luxury but a core professional obligation.
From the perspective of career development within the helping professions, the dispatcher’s role presents a compelling model of transferable competence and lifelong growth. The ability to stay calm, to manage information under time pressure, and to coordinate multidisciplinary teams translates well into many other allied fields—from crisis counseling to community health education, from emergency management to social services coordination. The dispatcher’s pathway often opens doors to leadership roles within the public safety ecosystem, where decision-making under uncertainty remains the central competency, but with greater scope and responsibility. Even as their primary work remains rooted in the emergency call, the skills they cultivate—the ability to listen, to ask precise questions, to interpret rapid shifts in a situation, and to preserve the integrity of data—are valuable in any context where helping others hinges on accurate, timely action.
For readers exploring the wider landscape of helping careers, consider this chapter as a lens on how service evolves in response to complexity. The broader field includes professionals who move between direct care and systems-level roles, and the dispatcher’s experience highlights how the human element remains central even as technology, protocols, and interagency collaboration expand what is possible. A practical way to situate this career among others is to view it as part of a continuum of helping roles that require resilience, communication finesse, and a commitment to the safety and dignity of those who seek aid. As you survey the different paths, you can see how the craft of helping is less about a single job title and more about the consistent demonstration of responsibility, presence, and the ethical use of information in moments that matter most. If you are curious about how such paths interconnect or where a background in assisting others can lead beyond the dispatch console, a useful overview of multiple helping careers is available here: 17-careers-for-helping-people.
The connective tissue between dispatch work and the wider field of helpers is the shared emphasis on service quality, continuous improvement, and the belief that even the smallest act—an attentive question, a precise message to responders, a moment of steady reassurance—can alter outcomes. In practice, this means that training programs are evolving to be more holistic. They incorporate cognitive psychology, communication science, and evidence-based protocols, while still honoring the core values of compassion and accountability that define the helping professions. The goal is not to produce technicians who follow scripts, but professionals who can think clearly under pressure, adapt to shifting realities, and preserve the trust that communities place in their public safety systems.
To appreciate the breadth of this field, it helps to look at how dispatchers are integrated with other health and safety professionals. When a call comes in, the dispatcher becomes the central node that aligns the needs of the caller with the expertise of responders on the ground. The speed and clarity of that alignment influence not only the immediate outcome but also the longer arc of a case—from the patient’s recovery trajectory to the eventual understanding of what happened and why. In this sense, the dispatcher’s role is both practical and philosophical: it is a craft of humane efficiency, a discipline that respects the reality of fear while insisting on the highest standards of accuracy and coordination. This balance is what makes the job deeply meaningful and, for many, a gateway to a career dedicated to helping others in diverse, meaningful ways.
As this exploration of 911 dispatchers reveals, the field stands at the intersection of human touch and systemic precision. The work demands a unique blend of listening, discernment, and decisive action, reinforced by ongoing learning that keeps pace with research and evolving best practices. The result is a profession that not only saves lives in the moment but also strengthens the ethical fabric of how communities respond to danger. For those drawn to careers where helpers are necessary, visible in the moment and yet always part of a larger story, dispatch work offers a compelling, impactful path—one that honors the core idea behind every helping profession: that care arrives as much through careful listening as through quick intervention. For a broader look at related helping careers and the variety of ways to serve, readers can explore the overview linked here: https://coffee-beans.coffee/blog/17-careers-for-helping-people/.
External resource: For a deeper understanding of standardized, evidence-based guidelines that shape dispatcher training and practice, see the National Emergency Number Association guidelines: https://www.nena.org.
Final thoughts
The professions highlighted in this article collectively represent a significant part of our societal infrastructure, each dedicated to enhancing the well-being of individuals and communities. As the demand for skilled helpers continues to rise, understanding the critical contributions of home health aides, personal trainers, paramedics, rehabilitation specialists, and 911 dispatchers becomes increasingly important. Business owners should recognize the value these careers add to our society and consider how they can support or engage with these professionals to foster a healthier, safer environment for everyone.