The diligence and commitment of numerous professionals are essential to maintaining life and safety in our communities. From first responders to healthcare heroes, they confront dangers head-on and make quick decisions that can mean the difference between life and death. Business owners should recognize these critical roles not just for their societal importance but also for the indirect ways these professions can impact workforce stability and community health. This article navigates the vital contributions of firefighters, emergency medical technicians (EMTs), surgeons, critical care nurses, public health workers, and medical researchers—highlighting their unique impact on saving lives.
Brave, Timely, and Ready: Firefighters at the Frontline Where Time Becomes Life
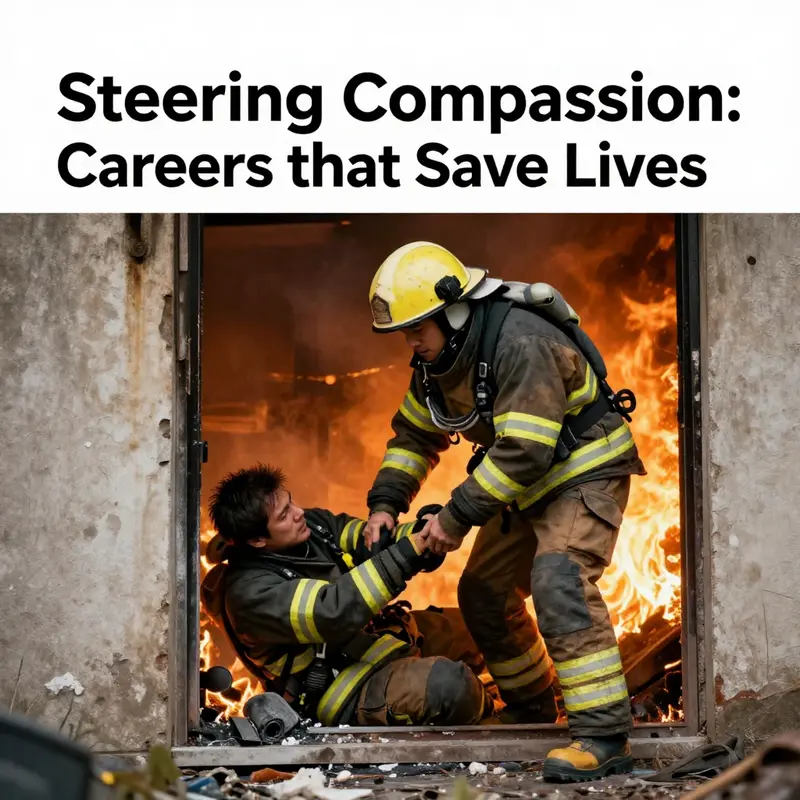
Firefighters are the frontline of emergency response, the people who confront danger so others can breathe a little easier. They enter scenes where the air is thick with smoke, heat, and fear, and they do so with a blend of skill, courage, and practiced coordination. Their work is not only about suppressing flames but about shaping outcomes—creating conditions in which lives can be preserved, families can be kept intact, and communities can begin to heal. The rhythm of a shift moves from alert to action in seconds. A call comes in, and within moments a crew slides into turnout gear, climbs into a cab, and turns toward a horizon that may change as the minutes pass. The job is a test of nerve and judgment, but it is also a discipline that turns danger into a sequence of controlled steps. Each flashover avoided, each life saved, adds a thread to the larger tapestry of public safety. The public often sees the majestic plume and the brave faces, yet behind the scenes is a complex system built on training, teamwork, and a relentless pursuit of mastery.
No two rescues look alike, and that variability is a constant reminder of why firefighters cultivate a broad, adaptable skill set. They learn to size up a scene in seconds, to read the signs that identify whether a stairwell is stable, whether a room is becoming a furnace, or whether a victim can be reached without creating a new hazard. The work requires precision under pressure, a calm voice in chaotic spaces, and a readiness to switch from suppressive tactics to rescue operations in the blink of an eye. It is a field where physical endurance and mental clarity must coexist, because a moment of tired judgment can have serious consequences for both the responders and those they aim to protect. Firefighters train not to perform heroic acts in isolation, but to operate as a tightly knit unit where every role supports another. A nozzle team, a search crew, a driver-engineer, and a incident commander each carry a piece of the mission, and the sum total is a coordinated cadence that maximizes the odds of survival for people who may have never met the responders before that moment.
Beyond the flames lies another dimension of the profession: the medical first response. Firefighters are often the first on the scene of medical emergencies, providing essential life support until paramedics take over. They assess airway, breathing, and circulation while delivering rapid care and stabilizing victims so that definitive treatment in a hospital can begin without delay. This intersection of fire suppression and medical intervention elevates firefighting from a purely tactical discipline into a comprehensive lifesaving science. It also underscores the importance of ongoing training that keeps responders prepared for illnesses and injuries that arrive in seas of smoke or the stillest of clinical quiet. The dynamic is relentless: the situation demands quick, accurate decisions, but those decisions must be informed by a breadth of knowledge that spans rescue techniques, triage principles, and safe patient handling. The result is a form of practice that blends science with the art of human care, where the aim is not to win a scene by force but to secure life through disciplined, compassionate action.
The gear that makes this possible is both legendary and highly practical. Modern firefighters move through environments that would overwhelm the untrained: heat, flames, toxic fumes, and unstable structures. They rely on self-contained breathing apparatus, fire-resistant turnout gear, helmets, gloves, and boots, all crafted to withstand extreme conditions. Yet gear is only as good as the way it is used. Teams rehearse every maneuver in training yards and simulated scenarios until their movements become almost automatic. The rhythm of a rescue hinges on communication and trust: a call sign, a plan, a backup plan, and a readiness to adapt if conditions shift. Even in the most controlled drills, the risk remains, which is why material safety expectations and equipment checks are woven into the fabric of daily life in the firehouse. The discipline of maintenance—inspecting hoses, testing pumps, verifying air supply—ensures that when a real emergency occurs, the tools function as expected and the team can focus on the human element of the mission rather than on equipment failures.
Climate change has intensified the tempo and scale of their work. Wildfires in certain regions expand into longer seasons and danger zones, threatening homes, ecosystems, and air quality for neighboring towns. Firefighters have responded by strengthening mutual aid networks, investing in faster, more durable equipment, and adjusting deployment strategies to address shifting risk landscapes. They also participate in prevention outreach, advising communities on defensible space, building codes, and evacuation planning. These efforts extend the life-saving reach of the profession beyond the immediate rescue, weaving prevention, preparedness, and rapid response into a holistic public-safety approach. In places where the smoky skies loom for weeks and the terrain favors flames over chance, every firefighter carries the burden and the reward of protecting not just one life, but entire neighborhoods that would otherwise face catastrophic losses. The bigger narrative here is that saving lives in an era of climate uncertainty demands not only bravery but also adaptability, collaboration, and a willingness to reimagine how communities defend themselves against hazards that are growing more complex.
Inclusivity has also evolved the field. The language around the profession has shifted toward gender-neutral terminology, and the result is more accurate, inclusive storytelling about who can serve and how. The term firefighter, favored for its inclusivity, reflects a culture that values capability over stereotype and recognizes that the courage to run toward danger does not belong to a single background. This shift helps recruit a diverse workforce whose varied experiences strengthen problem-solving on the ground. It also broadens the pool of people who can imagine themselves in a role that makes a direct, measurable difference in lives—whether they come from rural townships or sprawling metropolitan districts. The human dimension remains central: the courage to face uncertainty, the empathy to support frightened families, and the resilience to return to the firehouse after moments that tested every fiber of one’s nerves.
Public recognition for firefighters often comes in rituals, anniversaries, and moments of media attention that spotlight a dramatic save. National Fire Prevention Week, for example, keeps prevention in the public eye and reminds communities that protection begins with education and simple safety habits. The profession is likewise punctuated by stories of cross-border cooperation and shared purpose. A recent instance highlighted the steadfast collaboration between firefighting teams in different jurisdictions who coordinated in the face of a large-scale incident near a border region. Such narratives illustrate a universal truth: when lives hang in the balance, skill and trust transcend borders and politics, and the common goal of saving lives binds people across lines of difference. These moments reinforce why the path into firefighting, while demanding, is profoundly meaningful to those who choose it and to the communities they serve.
The work exacts a heavy toll, and responsible departments recognize the importance of mental health and ongoing support for responders. The emotional weight of witnessing trauma, the physical strain of carrying heavy gear through perilous conditions, and the sheer tempo of back-to-back calls all contribute to what many describe as the hidden cost of saving lives. Fire departments increasingly emphasize peer support, access to counseling, and structured decompression after intense incidents. This commitment to the well-being of the responders themselves ensures that those who save lives can continue to perform under pressure with clarity and care. It also sends a powerful message that courage includes seeking help when needed and that asking for support is a sign of strength, not weakness. In this way, the profession models a healthier culture that sustains both the individuals and the communities they defend.
For those considering a path toward such a role, the journey starts with a foundation in physical fitness, technical training, and a mindset oriented to service. Many departments require certification that encompasses fire suppression, rescue, and medical response, alongside ongoing training to stay current with evolving standards. The arc toward mastery is not a solitary ascent; it unfolds in a firehouse that functions as a classroom, a workshop, and a home away from home. Mentors, drills, and real-world calls reinforce practical knowledge while shaping professional identity. As aspiring firefighters study movement, chemistry, and anatomy in the context of real emergencies, they learn to translate theory into action—how to improvise when resources are limited, how to maintain composure when rescue hinges on a breath held in the direction of a dangerous corridor, and how to communicate a plan clearly so that every teammate can follow without hesitation. In this sense, the discipline is as much about character as it is about technique.
Within the broader landscape of lifesaving careers, firefighters occupy a critical niche that complements medical trauma teams, search and rescue specialists, and public health defenders who work behind the scenes to prevent harm. For readers exploring the spectrum of opportunities to save lives, a consolidated overview such as the article 17-careers-for-helping-people can provide valuable context about how distinct paths share a common commitment to safeguarding others. It is a reminder that every role—whether on foot, in the air, or within a hospital corridor—contributes to a safety net designed to preserve life and dignity. The chain of care, from prevention to immediate response to recovery, depends on the seamless integration of diverse skills and communities working in concert. Firefighters exemplify how courage, preparation, and cooperation can translate into life-sustaining outcomes when seconds count and hope hangs in the balance.
In closing, the story of firefighting is not only about extinguishing flames but about maintaining a culture of readiness, resilience, and respect for life. It is about the quiet confidence that comes from training that never stops and from teamwork that never falters. It is about the willingness to stand at the threshold of danger so that another person may pass through to safety. This is the essence of being a lifesaver on the front lines—the daily commitment to convert fear into action, uncertainty into control, and peril into the next breath of life. For communities, that is the quiet assurance that while hazards may come, the people who answer the call—and the system that supports them—will stand ready when time becomes life. External resource: NFPA
First on the Scene: Lifesaving EMTs and Paramedics on the Frontline
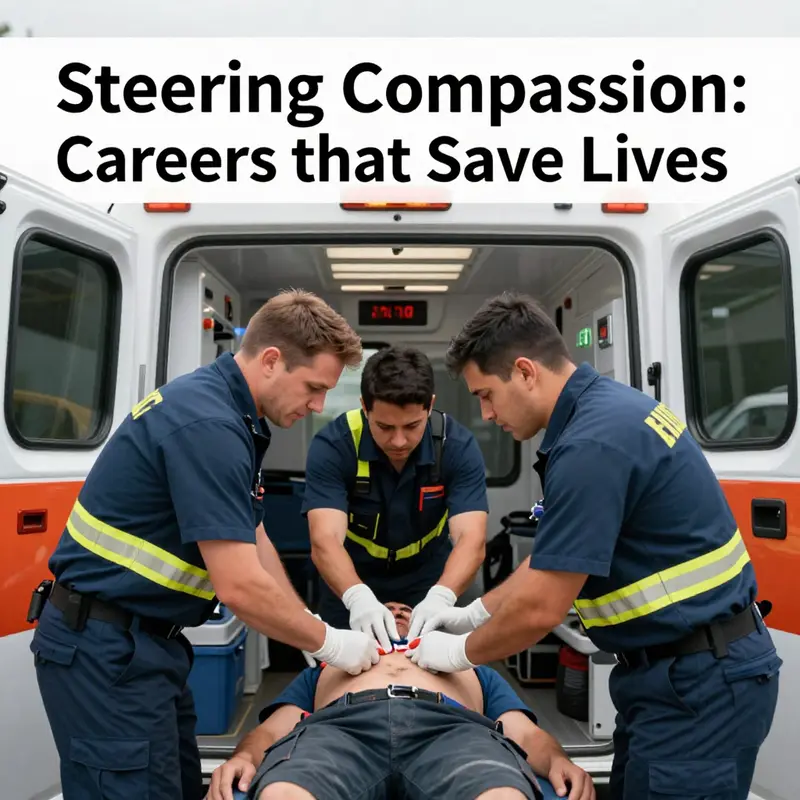
The moment the siren cuts through the night, EMTs and paramedics move with practiced calm, each action deliberate to stabilize a patient, secure an airway, control bleeding, and prepare for transport. They are both scientists and storytellers, translating vital signs into clear choices and communicating with families who cling to hope. Training spans basics to advanced life support, and across countries the core mission remains: deliver high quality care as the first link in a long chain of survival, from on scene care to definitive treatment, while collaborating with dispatch, fire services, hospital teams, and public health partners.
Beating at the Center: How Surgeons and Critical Care Nurses Drive Life-Saving Medicine
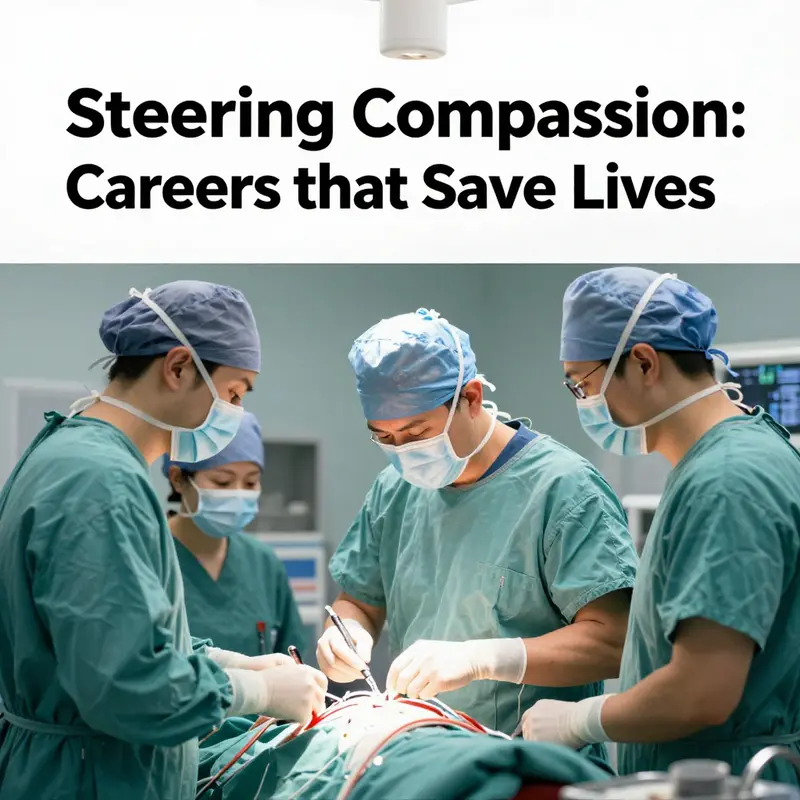
In the quiet, tense minutes that determine outcomes, and in the long, tired hours that follow, the operating room and the intensive care unit form a single, life-sustaining loop. Two professional cultures—surgeons and critical care nurses—provide a seamless rhythm that can convert a crisis into a recovery. They stand at the center of modern medicine, where intervention is both precise and compassionate, where the patient’s chances hinge on timely decisions and steady hands, and where every action is tethered to the broader goal of preserving life. The image of a surgeon’s scalpel gleams with technical mastery, yet it is the accompaniment of a critical care nurse’s vigilance that often makes the critical difference between a fragile stability and a sustained recovery. Together, they create a clinical choreography that keeps vital systems in balance long enough for healing to begin and for bodies to regain their capacity to fight anew against injury or disease.
The surgeon’s role is multidimensional and exacting. It begins with diagnosis and planning, evolves into assessment during an operation, and extends into decisions about postoperative care that determine whether a patient will wake from anesthesia, tolerate a procedure’s aftereffects, or emerge with restored function. Surgeons address acute injuries and bodily failures that threaten life: ruptured arteries, obstructed blood flow, complex trauma from accidents, the rapid labyrinth of cardiac events, or the invasive steps needed to remove malignant growths. Each operation carries risk, and the surgeon’s responsibility is to minimize that risk while maximizing the patient’s odds of a meaningful recovery. The craft requires not only dexterity but the ability to interpret physiological signals in real time, to anticipate complications, and to adjust plans when the body does not follow the expected script. In high-stakes moments, the margin for error narrows, and precision becomes the language through which hope is translated into outcomes.
Critical care nurses perform a counterpoint to the surgeon’s decisive interventions: they translate intent into ongoing, life-sustaining care once the patient leaves the operating table or arrives in the ICU with fragile physiologies. Their work is continuous and nuanced. They monitor vital signs as if they are listening to a patient’s breath between each heartbeat, recognizing the subtle shifts that might herald danger. They administer medications, adjust fluid balances, manage complex technologies like ventilators and infusion pumps, and respond rapidly to changes in a patient’s condition. The tempo of the ICU is relentless, but it is guided by a nurse’s trained judgment that blends science with empathy. When a patient’s condition deteriorates, it is often the critical care nurse who notices the earliest signs, documents the trajectory, and mobilizes the team to intervene—sometimes within seconds, sometimes within minutes, always with the patient’s best interests in mind.
This partnership operates within a shared language of urgency, but it also depends on a cultivated culture of collaboration. The surgeon sets the overarching plan and the critical care nurse keeps the patient on that plan’s rails. The nurse’s day-to-day responsibilities require meticulous attention to a patient’s evolving needs: adjusting medications, ensuring adequate oxygen delivery, and preventing complications such as infection, fluid overload, or delirium. The surgeon’s decisions—whether to proceed with a repair, to modify an approach, or to escalate to a more complex intervention—rely on the nurse’s observations and the team’s consensus about timing and risk. In warm, human terms, both professionals align their instincts with the patient’s values and goals, a task that is not merely technical but deeply ethical. The result is care that is as much about safety and dignity as it is about a restorative procedure.
The evidence that binds surgeons and critical care nurses into this vital pair comes from both clinical outcomes and the lived experience of those who work in the high-stakes domains of surgery and intensive care. Inagaki’s 2023 exploration of the dynamics between nurses and surgeons highlights something essential: the perceptions and contributions of nurses are not peripheral to patient safety but central to it. When nurses are engaged partners—sharing concerns, contributing to decisions, and communicating clearly with families—the healthcare team navigates complex situations more securely. This collaborative posture reduces the likelihood of communication breakdowns, shortens delays in recognizing deterioration, and supports more timely and appropriate interventions. The synergy is not about hierarchy but about a shared responsibility to protect life and promote recovery in the most vulnerable moments. In practice, this translates into safer care pathways, fewer preventable complications, and smoother transitions from the operating room to the recovery unit and beyond.
The day-to-day reality of this collaboration can be seen in how rounds unfold, how handoffs are conducted, and how information is shared with families. Effective rounds bring together surgeons, critical care nurses, respiratory therapists, pharmacists, and, when needed, ancillary specialists such as perfusionists or neurologists. Each voice adds a piece of the puzzle, and each piece helps to produce a fuller picture of the patient’s status. When a nurse reports a subtle but concerning change—an early sign of respiratory compromise, a fluctuating blood pressure, or a change in mental status—the surgeon must decide whether to adjust the surgical plan, to intensify monitoring, or to intervene more aggressively. The nurse’s perspective becomes part of the diagnostic tapestry, the same way a radiograph or a lab value would. Shared decision-making extends beyond the bed to include families who must understand options, risks, and expected trajectories. This is where ethical care and compassionate communication converge, offering families a sense of partnership and hope even in the face of critical illness.
The importance of this collaborative spirit is not merely theoretical. It influences patient safety and recovery trajectories in tangible ways. When surgeons and critical care nurses work as a coherent unit, patients experience more stable hemodynamics, quicker identification of complications, and more timely escalation of care when needed. The nurse’s role in monitoring and early warning detection often anticipates problems before they require emergent surgery or ICU escalation, while the surgeon’s ability to implement corrective interventions when indicated can reverse life-threatening trajectories. The resulting care is comprehensive and continuous, not episodic—a sequence of interventions that respects both the body’s needs and the patient’s values. This is the core of life-saving medicine: a dynamic, patient-centered partnership that remains attuned to the person behind the clinical condition.
Within this framework, the broader health-care ecosystem matters as well. Interdisciplinary collaboration—between surgeons, critical care nurses, pharmacists, physical therapists, social workers, and others—creates the scaffolding that supports not only survival but long-term recovery and quality of life. The interlocking roles extend beyond the operating room and ICU, shaping decisions about rehabilitation, discharge planning, and family support. In practical terms, a patient recovering from major cardiac surgery benefits from a nurse who can anticipate the needs of early mobilization, a physical therapist who can tailor a safe plan for movement, and a dietitian who can support heart-healthy nutrition. Each professional’s expertise informs the others, and each informs the patient’s pathway toward independence.
For readers curious about how this cross-professional collaboration translates into everyday practice, consider the broader literature that examines how different health disciplines coordinate care. One facet of this collaboration is the formal integration of patient values and family preferences into treatment decisions. The emphasis on patient-centered care, shared decision-making, and ethical communication is reflected in studies that show improved safety outcomes when teams align around the patient’s goals. This alignment does not reduce the surgeon’s responsibility or the nurse’s vigilance; instead, it sharpens the focus of both roles toward what matters most to the patient—survival with dignity and a viable path to recovery.
The narrative of two professions working as one is also a narrative about continuous learning and adaptability. The environment of critical care is constantly evolving: new monitoring technologies, evolving surgical techniques, and evolving best practices require ongoing education and flexible teamwork. Simulation training, interdisciplinary case reviews, and reflective practice are not mere add-ons; they are essential mechanisms that strengthen safety culture, reduce preventable errors, and enhance the collective ability to respond to unforeseen challenges. When surgeons and critical care nurses train together, they grow a shared language and a shared sense of timing. In moments of crisis, this cohesion translates into decisive, coordinated action that preserves life and supports recovery.
The interplay between technical prowess and relational skill is at the heart of what makes life-saving interventions possible. The surgeon’s skill can repair a ruptured vessel, remove a life-threatening lesion, or implement a complex reconstructive strategy. The critical care nurse’s skill can stabilize physiology, prevent secondary complications, and sustain the patient through the most fragile hours of recovery. The most compelling clinical stories emerge when these talents converge in real time: a surgeon adjusts a plan in response to a nurse’s observation; a nurse voices concern about a subtle trend in vital signs and the team pivots to provide targeted support; a family member, counseled with empathy, makes a decision that aligns with the patient’s previously stated wishes. These moments reveal medicine at its best—technical excellence married to compassionate care, with patient safety as the shared horizon.
As the field advances, the emphasis on collaboration grows clearer. The hospital environment that supports life-saving interventions is one that values the nurse as a partner with standing expertise, not merely as support staff. It is a culture that invites nurses into the decision-making conversations that shape outcomes, acknowledging that their closer proximity to patients’ daily realities yields insights that can prevent deterioration and guide timely actions. The same is true for surgeons: acknowledging the nurse’s expertise, listening to team members’ concerns, and adjusting plans in light of collective wisdom all contribute to better survival rates and more meaningful recoveries. This reciprocal respect and shared responsibility lie at the core of what makes life-saving medicine possible in high-stakes settings.
The practical implications of this partnership extend beyond the operating room. They influence how health systems are organized, how teams are trained, and how care pathways are designed to support patients through the most fragile phases of illness. When care is organized around the patient’s trajectory rather than around rigid departmental boundaries, the chances of timely intervention improve. The patient’s journey becomes a narrative of coordinated care, with surgeons and critical care nurses guiding the course, supported by a wider team that shares the goal of preserving life and optimizing recovery. The result is a healthcare experience that is not only technically proficient but also ethically attentive and emotionally attuned to families and communities.
In this movement toward integrated care, the value of cross-disciplinary collaboration is increasingly recognized in professional development and research. It is a reminder that life-saving medicine is not the product of a single genius or a single specialty; it is the outcome of a disciplined, collaborative practice that respects the unique contributions of each member of the care team. The heart of this practice beats strongest where there is alignment between intention and action, between the surgeon’s decisive interventions and the nurse’s vigilant care, and between the patient’s needs, the family’s hopes, and the care team’s professional dedication. That alignment is the stable axis around which life-saving outcomes revolve, a reminder that the central act of medicine is always a collective act.
To reflect on the importance of this collaboration in more practical terms, readers can explore discussions of interdisciplinary partnerships in healthcare. This particular article highlights how different professionals collaborate to support patient care and how such collaboration can be translated into everyday practice across specialties. It serves as a reminder that improving patient outcomes is a shared enterprise, built on clear communication, mutual respect, and a shared commitment to the patient’s best interests. For readers seeking a direct route to broader conversations about teamwork in medicine, you can explore the concept of cross-disciplinary collaboration here: how occupational therapists collaborate with other healthcare professionals.
In sum, surgeons and critical care nurses sit at the beating heart of modern life-saving medicine. Their collaboration shapes every moment from the preparation of an operation to the careful management of a patient’s recovery. It is a partnership that blends the swift decisiveness of surgical intervention with the patient-centered vigilance of critical care nursing. It is a testament to what medicine can achieve when expertise is paired with empathy, when technical skill is matched by attentive care, and when a shared commitment to life sustains the patient through moments that could otherwise prove fatal. The chapter of life-saving intervention is written not by any single hand but by a coordinated, compassionate team whose combined actions preserve life, restore function, and honor the dignity of persons at their most vulnerable.
For those who wish to delve further into the science behind how such teamwork translates into safer, more effective care, consult broader literature on critical care nursing and surgical collaboration. A foundational resource discusses how nurses contribute to patient safety and outcomes in high-acuity settings, reinforcing the themes above and offering a framework for ongoing improvements in practice. You can access a detailed exploration of the role of critical care nurses and their impact on patient outcomes at this external resource: https://www.ncbi.nlm.nih.gov/books/NBK572469/.
Behind the Front Lines: How Public Health and Medical Research Save Lives at Scale
Public health workers and medical researchers operate in a space that often feels distant from the dramatic rescues and rapid interventions that capture headlines. Yet the lives saved by these roles are counted in longer arcs and broader populations. They build the foundations of safety, prevent harm before it happens, and arm clinicians with knowledge and tools that make every patient encounter more likely to end well. In many ways, these professionals are the quiet architects of life-saving outcomes, weaving prevention, discovery, and policy into a fabric that protects communities day after day. When we think about jobs that save lives, the frontline heroes who sprint into burning buildings or perform lifesaving surgeries come to mind first. But the work of public health workers and medical researchers shapes the entire ecosystem in which those front-line acts occur. Their influence is cumulative and systemic, less dramatic at the moment of action but decisive in the outcomes that follow.
Public health workers stand at the intersection of science, policy, and community life. Their contributions begin with prevention—measured, data-driven, and relentlessly pragmatic. Infection control, one of their most visible domains, is a case study in how prevention saves lives on a population level. When hospital teams have reliable protocols, when healthcare workers are trained to don and doff protective gear correctly, and when surveillance systems detect a trend before it becomes a surge, lives are protected long before patients reach the emergency department. The lessons from past crises—the PPE shortages and gaps in training that amplified risk—have sharpened the public health playbook. The result is not only better patient outcomes but also more resilient health systems that can absorb shocks, whether from an influenza season, a localized outbreak, or a natural disaster. Strengthening public health infrastructure, including training and dependable PPE supply chains, is not a luxury; it is a core life-saving intervention that reduces exposure, lowers mortality, and speeds recovery for whole communities.
Equally central is the work of public health in addressing health equity. The most effective prevention strategies are those that reach everyone, including people in underserved neighborhoods, rural areas, and marginalized groups who often bear the heaviest burden of disease. This is why conversations about health equity, as reflected in authoritative public health resources, matter. A system that monitors who benefits from vaccination programs, who has access to clean water and safe housing, and who faces environmental risks is a system designed to prevent deaths that could otherwise occur in the margins. Public health professionals translate data into action, shaping outreach, education, and resources so that protective measures are not a privilege but a standard.
Within this field, long-term systemic challenges demand continuous attention. Equitable access to care, environmental health risks, and the management of chronic diseases are not episodic problems; they are part of a steady drumbeat that can determine life expectancy and quality of life. Consider chronic kidney disease, for example, where safe and sustainable dialysis infrastructure touches tens or hundreds of thousands of patients. The governance and design of those systems require the collaboration of engineers, policymakers, clinicians, and community advocates. Public health professionals, by coordinating these efforts, ensure that lifesaving therapies are not only available but delivered with dignity and consistency. In this broader frame, the goal becomes not simply to treat illness but to prevent it where possible and to mitigate its most dangerous consequences where it cannot be prevented.
Medical researchers occupy a complementary space that amplifies the impact of frontline care. Funded largely by institutions like the National Institutes of Health in the United States and equivalent bodies around the world, medical research is the engine behind vaccines, therapies, and improved diagnostic tools. The argument for sustained, robust research funding is not a theoretical one. Cardiovascular disease, infectious diseases, cancer, and many other conditions—each responsible for thousands of deaths daily—are gradually tamed through decades of meticulous study. This is not about glamorous breakthroughs alone. It is about the steady, often incremental work of labs, clinical trials, and data analysis that create the next generation of interventions.
A central point in this narrative is that the funds flowing to medical research support far more than laboratories. NIH and similar agencies provide essential institutional resources: laboratory infrastructure, administrative support, shared equipment, and the training capacity that allows scientists to push ideas from concept to clinical reality. Without this foundational support, the most promising discoveries would stall, and patient lives would wait longer for beneficial therapies. Critics sometimes frame research funding as a sunk cost, but experts argue that such investments yield a multiplier effect in health outcomes, economic stability, and national resilience. The lives saved through vaccines, optimized treatments, and preventive strategies are the visible surface of a much larger, often unseen, ecosystem of support and collaboration.
This ecosystem operates across dozens of disciplines and sectors. Epidemiology and biostatistics illuminate how diseases move through populations, enabling timely interventions. Health policy and management translate findings into scalable programs that reach clinics, schools, workplaces, and homes. Community outreach translates science into action, tailoring messages to local languages, cultures, and realities. In this way, public health and medical research do not merely add years to life; they improve the quality of those years by reducing the suffering associated with preventable illness, disability, and death. The collaboration between researchers, clinicians, and public health practitioners creates a safety net that catches people at every point in the health continuum, from the first signs of a potential outbreak to the long-term management of chronic conditions.
The role of prevention in saving lives inevitably intersects with policy, funding, and workforce development. A healthy research environment requires trained professionals who can design studies, manage data, and advocate for necessary resources. In many countries, concerted efforts to develop the public health and research workforce are underway, with institutional and governmental commitments designed to strengthen resilience against future health threats. The intent is not merely to respond to crises but to anticipate them and to limit their human and social costs. As the research enterprise matures, it also becomes more inclusive: expanding opportunities for diverse populations to contribute to and benefit from scientific advances. Equitable participation in research not only improves study results but broadens the range of life-saving applications across communities.
For those drawn to a career path in this arena, the opportunities are varied and deeply meaningful. Public health and medical research offer pathways that span fieldwork, data analysis, policy development, and program implementation. The possibilities include epidemiology, biostatistics, health policy, community outreach, and translational science, among many others. A sense of purpose grows from knowing that one’s work helps prevent illness, shorten suffering, and extend lives on a population scale. It is a different repertoire of heroism than the dramatic rescue, yet it is no less consequential. It requires patience, collaboration, and a willingness to work behind the scenes where decisions are made, infrastructures are built, and futures are shaped. For those seeking concrete entry points, one helpful resource highlights a broad spectrum of roles devoted to helping others and making systems safer and more just. Explore 17 Careers for Helping People to gain a sense of how these fields translate into real-world impact and meaningful daily work.
The potential of these indirect, system-wide roles is hard to overstate. Public health workers and medical researchers do not always capture attention with dramatic headlines, but their influence is continuous and cumulative. They provide the steady push that keeps people healthier year after year, the early warnings that prevent outbreaks from spiraling, and the innovations that expand the boundaries of what medicine can achieve. In a global health landscape increasingly shaped by infectious threats, aging populations, and social inequities, the demand for skilled professionals in these fields continues to rise. Staffing, training, and sustained investment in public health and research become critical levers for saving lives in the present and ensuring a healthier horizon for the future.
This chapter would be incomplete without acknowledging the broader social contract that underpins these efforts. Public health and medical research depend on trust—from participants in studies to patients in clinics, from funders to policymakers. Maintaining this trust requires transparency, ethical governance, and a clear demonstration of value. It also calls for a vision that recognizes health as a shared resource, something that benefits everyone, not just a subset of the population. When communities see that their health data are used to protect them, when researchers share findings that lead to practical improvements, and when policymakers translate evidence into tangible programs, the cycle of protection strengthens. The result is a healthier society in which more people can live longer and with greater well-being.
The enmeshment of prevention, discovery, and equity frames the life-saving power of these indirect roles. Public health workers and medical researchers are not merely guardians against illness; they are architects of opportunity: opportunities for vaccination, early detection, effective treatment, and informed decision-making that respects patients’ values and contexts. They enable clinicians to do their work with better information, better tools, and better systems. They create the conditions in which life-saving care can be delivered quickly, equitably, and with compassion. That is the essence of why these careers matter so deeply to the mission of saving lives.
External resource: https://www.cdc.gov/healthyyouth/health_equity/index.htm
Final thoughts
The commitment displayed by firefighters, EMTs, surgeons, critical care nurses, public health workers, and medical researchers underscores the interconnectedness of the roles that save lives. These professionals not only confront emergencies but also lay the foundations for healthier communities through education and preventative care. Recognizing and supporting these careers is vital for the well-being of society. For business owners, understanding these crucial occupations can inspire workplace programs that promote health and safety, further fortifying the community in which we all thrive.