Occupational therapy (OT) is a vital service geared towards helping individuals regain their independence after injury, illness, or as they navigate disabilities. To achieve optimum outcomes, effective OT equipment is necessary. The following chapters delve into essential tools that facilitate rehabilitation, innovative equipment that enhances therapy, understanding the tangible outcomes from these tools, and future trends in OT equipment that can change lives for the better. Each chapter offers insights designed to equip business owners in the health industry with knowledge to make informed choices about the equipment they utilize or provide to their patients.
From Grips to Independence: The Subtle Craft of Therapy Equipment in Occupational Therapy
Occupational therapy is not merely a set of exercises or a list of devices. It is a careful orchestration of actions that connect a person’s abilities to the tasks that give life meaning—self-care, work, and play. In this light, therapy equipment becomes more than tools; it is a bridge between impairment and independence. When a therapist selects a grippable object, a pegboard, or a set of adaptive utensils, the choice reflects a precise understanding of how a client’s strengths, challenges, and daily routines intersect. Each piece of equipment is weighed not only for its mechanical demands but for the sensory, cognitive, and emotional responses it can provoke. The goal is to create opportunities for success in real-world activities, while also honoring the rhythms of the person’s body and mind. The result is a therapy that looks like everyday life but is crafted with deliberate expertise behind every grip, push, and turn.
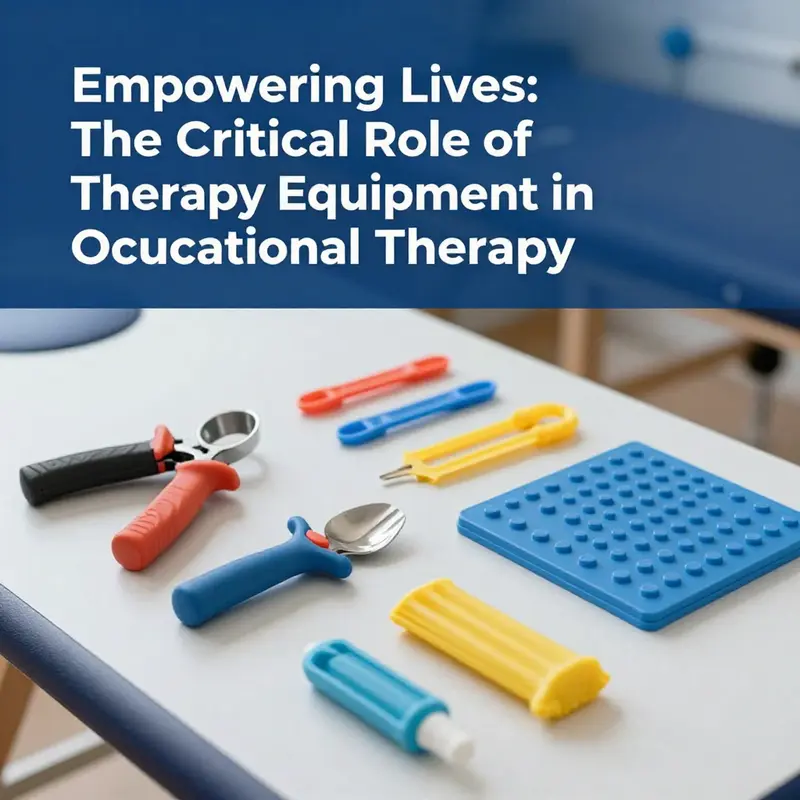
The conversation about therapy equipment begins with the body’s capability for movement and remains grounded in what a person needs to do to live independently. Fine motor skills—the small, exact motions of the fingers, hands, and wrists—often form the core challenge after injury or illness. Rebuilding these skills is not a single act but a sequence of small, purposeful steps. A grip strengthener, for instance, is not just about squeezing. It is about rebuilding a foundation of forearm endurance and hand control that supports a wider range of activities, from buttoning a shirt to opening a bottle or turning a doorknob. In the hands of a skilled OT, such tools are scaled to the person’s current level and gradually intensified as mastery grows. The patient learns to translate stronger grip into steadier handwriting, controlled tool use, and reliable dexterity in daily routines. This translation—turning bodily change into meaningful action—is the essence of therapy equipment in practice.
The story of the adaptive utensil set underscores a different strand of independence: eating. Large handles and weighted bases reduce the impact of tremor and limited dexterity, enabling a person to feed themselves with dignity. The difference between needing assistance and reclaiming autonomy often hinges on the details of the design. A handle that fits the average hand poorly becomes a barrier rather than a helper. By contrast, a thoughtfully shaped grip can transform a once-frustrating meal into a sequence of simple, confident motions. The same principle applies to other near-ubiquitous tools—the peg boards and lacing cards that address upper-limb coordination and fine motor control. They look simple, almost childlike, yet they rehearse the precise coordination required for tasks like assembling a routine, fastening shoes, or threading a needle. The patient’s fingers learn to choreograph their movements with increasing speed and accuracy, and the therapist reads subtle shifts in technique to decide when to introduce a new level of challenge or to provide supportive feedback.
In practice, therapists often weave these activities into meaningful, goal-centered routines. The sensory and perceptual demands of daily life—recognizing shapes, ordering objects, tracking sequences, and solving problems—are foundational to independence. For cognitive and perceptual training, sorting trays and pattern recognition puzzles offer a quiet but powerful way to rebuild attention, planning, and flexible thinking. These tasks translate into broader competence, such as organizing a kitchen space, managing a personal calendar, or completing a work-related procedure with fewer errors. The aim is not mere task repetition but the cultivation of cognitive strategies that persist beyond the therapy session. Sensory systems also come into play in everyday contexts, where a regulated nervous system makes learning and performance more efficient. Here, tools like therapeutic putty extend beyond grip work. Resistance-based exercises provide tactile feedback that stabilizes proprioception and enhances hand awareness, connecting physical effort with a clearer sense of how the body is aligned in space. The result is a cycle: sensory input informs motor output, and deliberate practice with the equipment refines both.
Sensory integration remains a core pillar of OT equipment. Weighted blankets, for instance, deliver deep pressure input that can calm an overreactive nervous system and sharpen concentration for task performance. This is not a luxury but a practical strategy—an enabling step before complex activities like meal prep, handwriting, or self-care routines. Textured sensory boards invite exploration, inviting hands to experience varied surfaces that stimulate the sense of touch while supporting modulation and engagement. Vibration toys add proprioceptive feedback that helps a person become more aware of their body in space, an awareness that frequently improves coordination and reduces anxiety during challenging tasks. Sensory bins filled with rice, beans, or sand create a multisensory play and learning environment. They offer a receptive space in which a client can explore textures, resistive forces, and timing—all while building tolerance for new experiences. Taken together, these tools form a regulated sensory platform in which goal-directed activities can flourish, turning regulation into a resource rather than a barrier to progress.
Fidget toys often populate the OT toolkit because they offer compact, portable means of addressing attention difficulties and self-regulation. A child with ADHD, or an adult coping with anxiety, can benefit from small, controllable tasks that provide sensory grounding and a sense of control. Yet the use of fidget objects requires careful judgment. The same devices that support focus can become a distraction if relied on inappropriately or left unchecked within a classroom or work setting. A thoughtful clinician will calibrate the texture, resistance, and noise level to the person’s age, setting, and goals, and will educate caregivers or employers about appropriate use. Safety considerations are essential: small parts can pose choking hazards for younger clients, and paths to overreliance must be avoided by pairing fidget work with structured, purpose-driven activities. When used judiciously, fidget tools become a bridge that links sensory modulation with sustained engagement, creating a more resilient platform for learning and performance.
Another important category is wearable chewable jewelry, designed to provide safe oral sensory input for individuals who seek sensory stimulation or who experience anxiety. Made from food-grade silicone, these items respond to oral-seeking behaviors without the risks associated with non-food objects. They help regulate arousal, support calm decision-making, and reduce stress during challenging routines. The risk-benefit analysis for such devices is nuanced. The clinician must assess age appropriateness, the client’s sensory profile, and the social context in which the tool will be used. When correctly matched to need, chewable jewelry can lessen self-soothing through unsafe chewing and provide a reliable, hygienic means of self-regulation that supports continued participation in meaningful activities. The full value of these tools emerges when they are integrated into intentional routines rather than used as ad hoc distractions. The clinician’s task is to embed them in tasks that matter to the client—self-care, school tasks, or work duties—so that regulation supports rather than interrupts daily life.
The narrative arc of OT equipment continues with precision tasks that train the fingers and the eyes to work in harmony. Peg boards and lacing cards, for example, challenge the hand’s precision and finger isolation, while requiring careful planning, sequencing, and bimanual coordination. Practicing these tasks not only strengthens the small muscles of the hand but also simulates the careful manipulation demanded by real-world activities, such as fastening buttons, threading lace into eyelets, or aligning hardware accurately in a repair or craft task. The beauty of these tools lies in their adaptability. They can be scaled to different ability levels and integrated with functional activities that reflect a client’s own interests, making therapy feel less like a clinical drill and more like purposeful play that yields practical outcomes. In this sense, the equipment becomes a language—one that translates therapy into tangible, transferable skills.
Among the most common goals in occupational therapy are building independence and expanding participation. A patient who gradually increases their independent eating, dressing, writing, or navigating public spaces is not simply performing exercises; they are rewriting the script of daily life. The adaptive utensils, peg boards, and other devices act as both scaffolds and motivators, lowering the barrier to entry for difficult tasks and providing a clear path toward mastery. Each session is an opportunity to adjust the fit and complexity of the tools so that the client experiences success at the edge of their current capability. The therapist pays attention to subtle shifts in grip, posture, and strategy. Small changes—a slightly larger handle, a different texture, or a gentler resistance—can result in meaningful progress. Through careful calibration, therapy equipment supports a streamlined trajectory from struggle to competence, from hesitation to confident action, and from dependence to increasing autonomy in everyday life.
The body of evidence supporting the use of therapy equipment is robust and continually evolving. The American Occupational Therapy Association highlights that evidence-based interventions using such tools significantly improve functional outcomes across diverse populations, including children with developmental delays, adults after stroke, and older adults facing age-related decline. Those findings reinforce the clinician’s clinical intuition: equipment is not a gimmick but a well-founded component of comprehensive rehabilitation. When used thoughtfully, these tools enable meaningful participation, reduce frustration, and empower clients to achieve goals that matter to them—whether that goal is to prepare a meal, manage personal care, or contribute to a workplace task. The chapter on essential tools in therapy equipment for occupational therapy thus serves as a reminder that the craft of OT lies in translating sensory, motor, cognitive, and emotional needs into practical strategies that restore independence and a sense of capability. The most effective clinical practice is not about racing through a checklist of devices but about building a coherent, personalized program in which every piece of equipment has a clear purpose and a measurable path to real-life outcomes. For a deeper dive into the practical guidelines and standards that shape this field, see the resource linked below and consider exploring related discussion on our site through the internal guide referenced here: tools-and-equipment-for-occupational-therapists. This is not merely a shopping list; it is a map to a more capable everyday life for clients of all ages and abilities.
In addition to the internal guidance above, the profession continually reinforces its commitments through external resources and ongoing research. The body of evidence from professional bodies and clinical practice demonstrates that when therapists tailor equipment to the individual and the task, functional outcomes improve across a broad spectrum of needs. The practices described here reflect a holistic approach that values safety, accessibility, and person-centered goals. They also acknowledge the importance of ongoing assessment, adaptation, and collaboration with caregivers, teachers, employers, and other health professionals. As clients progress, the therapy plan can evolve, introducing new challenges or refining existing tools to align with goals such as returning to school, re-entering the workforce, or enjoying leisure activities with greater independence. This dynamic, responsive approach is what makes therapy equipment integral to meaningful occupational therapy. External guidance and peer-reviewed research continue to inform practice, ensuring that equipment choices remain aligned with current standards and best practices. For those seeking broader standards and evidence-based guidelines, the American Occupational Therapy Association provides a foundational reference that supports the judicious use of equipment in diverse clinical settings. External resource: https://www.aota.org/.
Bridging Everyday Life and Therapy: The Evolving Landscape of Equipment in Occupational Therapy

In occupational therapy, equipment is more than hardware—it is a bridge between current abilities and daily life. OT equipment aims to restore or enhance independence in self-care, work, and leisure by supporting grip, dexterity, coordination, balance, and cognition. Therapists select and sequence tools to create sessions that feel purposeful and connected to real tasks. The field has evolved from simple devices to systems that simulate real-life activities with adjustable feedback, enabling tailoring to pace and goals. Modern equipment can model dressing, cooking, writing, and utensil use within a controlled setting, while offering immediate feedback and scalable challenges. Importantly, technology serves to augment the clinician’s judgment, providing data to monitor progress and guide progression. Equitable access remains a priority, with emphasis on safety, usability, and adaptability across diverse settings. Ultimately, equipment empowers people to reengage in daily life with confidence and dignity.
Harnessing Smart Tools: How Therapy Equipment Elevates Occupational Therapy Outcomes and Everyday Independence

Therapy equipment in occupational therapy is more than a collection of objects. It is a conduit for rebuilding the relationships people have with their daily lives. When a hand grinds to a halt after injury or illness, or when cognition shifts under the weight of aging or neurological change, the right tools can recalibrate the possibilities of daily self care, work tasks, and leisure. The equipment is not merely functional; it is a bridge between capacity and participation. A well-chosen set of tools supports a patient through a carefully paced journey from dependency to independence, a path that honors the complexity of human function. In modern practice, therapists blend traditional, hands-on therapies with intelligent rehabilitation devices to create treatment plans that are both grounded in everyday activities and informed by real-time data. This fusion allows clinicians to tailor activities to the person who uses them, rather than forcing the person to fit a standard exercise regimen. It is this person-centered, data-informed approach that drives meaningful gains in functional outcomes and life quality.\n\nThe old image of therapy being a steady stream of repetitive motions has given way to a more dynamic vision. Therapists select grip strengtheners to rebuild the force and endurance of the forearm and hand, adaptive utensil sets to restore autonomy at meals, and peg boards or lacing cards to refine eye-hand coordination. Each tool targets a specific facet of functioning, yet the most powerful outcomes emerge when these tools are integrated into purposeful activities. When a patient practices manipulating small objects, the action is not merely about dexterity. It becomes a rehearsal for a broader task: buttoning a shirt, threading a needle, or assembling a workstation at a future job. The same holds true for cognitive and perceptual tasks. Sorting trays and pattern recognition puzzles do more than entertain; they exercise attention, sequencing, and problem solving in contexts that resemble real life. Therapeutic putty, with its resistance and tactile feedback, can strengthen the hand while also offering sensory input that helps regulate arousal and focus. These materials, simple in appearance, act as multipliers for therapy sessions by providing varied, transferable experiences that translate to daily independence.\n\nYet the landscape of therapy equipment has expanded far beyond these traditional tools. Intelligent rehabilitation devices sit at the frontier, capable of capturing performance data, adapting difficulty in real time, and guiding therapy toward outcomes that matter most to each patient. The integration of technology with core occupational therapy principles creates a dynamic treatment environment. As patients work, sensors measure grip force, movement smoothness, reaction times, and task completion times. The therapist observes not only whether a task was completed, but how it was done: Did the patient use compensatory movements? Were there hesitations that suggested cognitive planning needed support? Were tremors or lapses in attention affecting performance? This data becomes a language that the therapist and patient share. It helps set priorities, adjust difficulty, and time progress so that practice remains challenging but achievable. The ability to observe, interpret, and respond in real time makes therapy more responsive to the patient’s actual pace of recovery rather than a fixed timetable that may overlook moment-to-moment fluctuations.\n\nFrom a clinical perspective, the value of intelligent devices lies in their ability to bridge the gap between laboratory precision and home-based practice. A session in clinic can be augmented by remote monitoring and guided home programs that echo the same therapeutic logic. When a patient returns to a kitchen task or workplace scenario, the same underlying principles apply: establish meaningful goals, plan the sequence of actions, execute with proper technique, monitor feedback, and adjust. The equipment is not a substitute for clinical judgment; it is the instrument through which clinicians translate that judgment into observable, measurable progress. Therapists use the data to confirm improvements in fine motor control, hand strength, and coordination, and to detect plateaus or regressions early. They also watch for shifts in cognitive performance, such as sustained attention and problem-solving efficiency, which are essential for independent living and employment. This synergy between human expertise and technological insight is at the heart of improved functional independence.\n\nTo illustrate how these tools function within the patient journey, consider how a therapist designs an intervention sequence. Early sessions might emphasize foundational strength through resistance-based activities, such as a therapeutic putty exercise or a controlled grip task that gradually increases in difficulty. The patient learns effective strategies for maintaining neutral wrist positions, stabilizing the forearm, and coordinating finger movements with the whole arm. As strength returns, clinicians introduce precision-demanding activities like peg boards or intricate lacing tasks. These tasks challenge dexterity and bimanual coordination while reinforcing the patient’s sense of accomplishment. Simultaneously, adaptive utensil sets become integral when self-feeding is a goal. Larger handles, weighted bases, and thoughtfully shaped utensils reduce the energy required for meals, enabling independent dining at home and in social settings. Each component of the toolkit serves a purpose, yet the real power emerges when they are orchestrated to reflect the patient’s living environment and daily rhythms. In this way, the equipment becomes a translator, converting clinical goals into practical capability that the patient can carry into the kitchen, the workstation, or the grocery store.\n\nIntelligent devices accentuate the storytelling aspect of therapy. Patients often reveal their values and priorities through the tasks they choose to pursue. By documenting progress through objective metrics, therapists can honor those priorities with concrete evidence of improvement. A patient who seeks to return to baking, for instance, benefits from precision hand movements while controlling grip force and wrist stability. The monitoring system might track how long it takes to pick up and place a small measuring cup or how accurately the patient pours without spilling. Over time, the data show that the patient can manage more delicate pours, handle heavier bowls, or complete more complex recipes with less support. This kind of progress is not only measurable but meaningful; it translates directly into a home environment where the patient can exercise independence, socialize more freely, and pursue valued activities without constant assistance.\n\nA critical advantage of equipment-based OT is its capacity to promote engagement and adherence. Therapists recognize that motivation drives outcomes as much as strength and coordination do. When equipment is aligned with the patient’s interests and daily routines, sessions become unlockable opportunities rather than abstract tasks. The use of gaming principles, scoring systems, and meaningful sequences can transform repetitive drills into purposeful practice. For some patients, the prospect of regaining a cherished hobby or resuming a rhythm of daily life provides intrinsic motivation that sustains effort across weeks and months. In this sense, therapy equipment acts as a facilitator of long-term adherence, helping patients integrate therapeutic activity into their everyday lives rather than treating therapy as a separate, temporary obligation. The most successful programs are those where therapy and daily life echo each other, creating a seamless continuum from rehabilitation to everyday competence.\n\nFrom a broader perspective, assistive technology and OT equipment collectively support not just recovery but participation. The literature increasingly points to outcomes that matter most to patients: independence with self-care, the ability to manage tasks at work or school, and the capacity to engage with friends and family without persistent reminders or assistance. The evidence base, including guidance from the American Occupational Therapy Association, underscores that evidence-based interventions using such tools can improve functional outcomes across diverse populations. Children with developmental delays, adults recovering from stroke, and older adults facing age-related changes all benefit when therapy designs incorporate appropriate equipment and intelligent feedback. The challenge for clinicians is to integrate these tools in ways that respect patient-centered goals while remaining sensitive to each person’s context, culture, and environment. This integration requires thoughtful selection, ongoing assessment, and a readiness to adjust in response to real-world use, not only clinical measurements.\n\nTo appreciate the practical implications of this approach, it helps to consider a clinician’s question about technology: what role does technology play in enhancing patient care in occupational therapy? The answer lies in a careful balance of capability, relevance, and humanity. Technology should amplify the therapist’s expertise, not replace it. Intelligent devices can take on routine data collection, freeing therapists to observe subtle changes in movement quality and to listen for patient narratives about shifting daily demands. They can model progress over time in a way that is accessible to patients and families, turning abstract improvement into tangible milestones. They can also reveal patterns that inform adjustments to home programs, scheduling, and environmental modifications. When used wisely, technology helps therapists personalize care while ensuring that each patient remains the central decision-maker in their rehabilitation plan. For readers who want to explore this topic further, the concept is well captured in discussions of the role of technology in enhancing patient care in occupational therapy, which offers a framework for aligning devices with meaningful goals and ethical practice. You can find more about this perspective here: the role of technology in enhancing patient care in occupational therapy.\n\nLooking ahead, the practice of occupational therapy will continue to evolve as tools become more capable and accessible. The ethical use of data, the need for patient-centered design, and the commitment to preserving the human touch in therapy sit at the core of this evolution. Clinicians must steward technology so that it serves people with diverse abilities and backgrounds, not the other way around. They must ensure that tools are adaptable to home environments, affordable for families, and compatible with community supports. They must also guard against overreliance on device-driven progress, recognizing that real-world independence emerges from a balanced combination of skill acquisition, strategy development, environmental modification, and social participation. In practice, this means harnessing the strengths of both hands: the therapist’s expert eye and the device’s precise feedback. It also means recognizing when a tool is not the right fit and offering alternatives that align with the patient’s values and daily routine.\n\nThe take-home message is simple and powerful: therapy equipment, especially when integrated with intelligent devices, can transform outcomes by making rehabilitation more personal, measurable, and connected to daily life. This is not mere optimization of exercise time; it is the cultivation of practical competence that carries patients beyond the clinic into a future of greater independence. As clinicians refine their approaches, patients experience therapy not as a distant goal but as an ongoing, engaged partnership that supports them in every ordinary moment—getting ready in the morning, navigating a workspace, sharing meals with loved ones, and pursuing activities that give life meaning. The equipment becomes a partner in that journey, a faithful ally that grows with the patient as they move toward fuller participation in the world around them.\n\nExternal resource: https://www.aota.org/-/media/Corporate/Files/Practice/OT-Technology-White-Paper.pdf
Smart Tools, Real-Time Feedback, and Home-Based Rehabilitation: Charting the Next Era of Occupational Therapy Equipment
The landscape of therapy equipment for occupational therapy is shifting from static aids anchored in clinic rooms to dynamic, data-driven companions that travel with patients into daily life. This transition is not merely a matter of adding gadgets to a toolbox; it reflects a deeper shift in how care is delivered, how progress is measured, and how engagement is sustained over the long arc of rehabilitation. Equipment is becoming a bridge between the controlled environment of therapy sessions and the unpredictable realities of home, work, and community life. In this evolving ecosystem, the patient is no longer a passive recipient of techniques but an active participant whose movements, choices, and outcomes are continuously observed, interpreted, and guided by intelligent, responsive tools. The implication for practice is profound: therapy becomes a continuous, adaptive dialogue between person and device, with the goal of building independence in self-care, productive work, and meaningful leisure.
Central to this new era is the integration of wearable technology and real-time biofeedback systems. Electromyography (EMG) biofeedback devices exemplify a trend toward making the body’s subtle signals visible and accessible. When a patient performs a grasp, reach, or release, EMG sensors translate electrical activity into immediate visual or auditory feedback. This feedback loop helps patients recognize and adjust motor patterns that may be inefficient or maladaptive. For conditions such as stroke recovery, orthopedic rehabilitation, or pelvic floor therapy, real-time feedback supports active participation and reinforces correct strategies. The portability of these systems means therapy can move beyond the clinic walls and into homes, schools, or workplaces, with data streaming to a therapist’s dashboard or mobile app. This remote, app-supported model reduces barriers of travel and scheduling while preserving the clinician’s ability to calibrate difficulty, set thresholds, and monitor adherence. Importantly, biofeedback encourages a growth mindset; patients see how small, precise adjustments lead to meaningful gains, which in turn nurtures motivation and persistence. The data stream also invites clinicians to detect plateaus or regressions early, enabling timely modifications to exercise dose, task complexity, or sequencing. In this context, the equipment itself becomes a collaborative partner—adaptive, responsive, and tuned to the individual’s pace and goals.
Augmenting physical practice, immersive technologies such as augmented reality (AR) and virtual reality (VR) are reshaping how patients rehearse daily activities in a controlled yet lifelike safe space. VR environments can simulate day-to-day tasks—cooking, dressing, managing a shopping trip, or navigating a familiar apartment—allowing patients to rehearse sequences, refine motor planning, and rehearse problem-solving strategies without fear of real-world consequences. For patients recovering from stroke, traumatic brain injury, or spinal cord injuries, this immersive rehearsal can accelerate reacquisition of complex, purposeful movements and improve cognitive flexibility in tandem with motor recovery. AR, by contrast, adds real-time visual overlays to the patient’s actual environment. This capability supports procedural guidance, environmental modifications, and assistive strategy coaching during tasks that would be difficult to simulate perfectly in VR. For therapists, AR and VR offer precise metrics on speed, accuracy, and error patterns, promoting data-informed decisions about progression and task selection. The benefit extends beyond clinical gains: patients often report greater engagement, reduced anxiety around challenging tasks, and a sense of empowerment as they master activities that once seemed out of reach. It is this blend of safety, immersion, and measurable progress that makes AR and VR compelling tools for OT practice, especially as cognitive and perceptual demands intersect with motor control in meaningful ways.
The rise of smart, interconnected devices equipped with artificial intelligence deepens the capacity for personalized care and long-term management. Modern therapy equipment increasingly incorporates data analytics and machine learning algorithms that can map a patient’s trajectory across weeks or months. These systems aggregate performance metrics from wearable sensors, EMG feedback, task completion times, error rates, and even sleep or stress indicators gathered through consumer devices. By identifying patterns, the algorithms can suggest adaptive treatment plans, alter task difficulty, or propose new activities aligned with the patient’s evolving profile. This capability is particularly valuable for chronic conditions and aging populations, where ongoing adjustment to therapy plans can prevent regression and promote preventive care. Yet as data streams expand, clinicians must balance technological insight with clinical judgment, ensuring that recommendations remain patient-centered and ethically sound. Interoperability with electronic health records and other care platforms becomes essential, enabling OT to coordinate with occupational therapists, physicians, and other professionals in a holistic, team-based approach. The potential market response is substantial: the global footprint of durable medical equipment is projected to grow as devices become more capable, connected, and capable of delivering value over time. For practitioners, the challenge lies in selecting tools that deliver meaningful data without overwhelming users or undermining the therapeutic relationship.
A parallel evolution is taking place in the design philosophy of therapy equipment: a shift toward personalization and prevention. No longer is equipment a one-size-fits-all proposition. The next generation of tools offers customizable settings, dynamic feedback thresholds, and patient-specific profiles that reflect an individual’s strength, endurance, cognitive load, and sensory preferences. This precision fosters more effective outcomes by ensuring tasks are challenging enough to elicit improvement but not so demanding that they trigger frustration or contraindicated efforts. For instance, a patient with tremor may benefit from adjustable weight and grip configurations that gradually reduce support as control improves. A patient recovering from anesthesia or a nerve injury might need explicit pacing and cadence cues, which can be tuned within an adaptive system. The preventive dimension emerges when these devices monitor subtle shifts in performance that precede relapse or overuse injuries, triggering preemptive adjustments, rest periods, or preventive strategies before problems escalate. This anticipatory approach aligns with broader health trends toward proactive care, where early intervention and consistent engagement reduce dependence on intensive clinician contact and help people maintain autonomy longer.
The practical implications of these trends extend beyond device features. They reshape how therapists plan sessions, how patients experience therapy, and how families and caregivers participate in rehabilitation. For therapists, the promise lies in more precise task analysis, richer feedback loops, and more efficient data collection that informs decisions about progression. The risk lies in cost, data security concerns, and the potential for technology to overshadow the therapeutic alliance if not used thoughtfully. The most effective practice will weave device-driven insights into an ongoing, responsive conversation with the patient, anchored in meaningful goals and daily life relevance. To realize this, education and ongoing professional development are essential. Clinicians must become proficient not only in traditional OT techniques but also in interpreting sensor data, managing software interfaces, and communicating progress in terms that are motivating to patients and understandable to families. Furthermore, training should emphasize cultural and cognitive accessibility so that devices support diverse populations without creating new forms of inequality.
Accessibility and equity remain central considerations as these technologies mature. The best-designed systems take into account varied home environments, access to internet connectivity, and user-friendly interfaces that accommodate different levels of digital literacy. For some patients, home-based rehabilitation may be a lifeline, enabling consistent practice when transportation or weather makes clinic visits impractical. For others, teletherapy-enabled OT can extend the reach of specialty expertise to rural or underserved communities. Equally important is the cost dimension. While the long-term value of engaged, data-informed therapy is clear, upfront investment and ongoing subscription costs can be barriers. Clinicians and program leaders must work with payers and policymakers to articulate the clinical and economic benefits of smart equipment, including reductions in hospital readmissions, improved function in daily activities, and enhanced independence at home. When pricing models align with real-world outcomes, patients are more likely to engage with durable, adaptive tools that support sustainable gains.
In this future-forward view, the role of the occupational therapy professional remains central. Technology acts as an amplifier of expertise, not a replacement for it. The therapist curates the selection of devices, interprets the data, translates information into actionable goals, and maintains the human-centered core of care. The patient’s lived experience—the everyday tasks that carry meaning, identity, and purpose—drives the choice of activities, the pacing of progress, and the interpretation of success. The equipment fosters a shared journey: the patient as the lead actor, the therapist as guide, and the tool as a reliable partner that records, reflects, and reinforces gains. As this trajectory unfolds, OT practice will increasingly balance the precision of analytics with the nuance of personhood, ensuring that advancement in therapy technology translates into tangible improvements in independence, quality of life, and the dignity of everyday living.
Readers may wish to explore further the broader implications for policy and practice as the market for durable medical equipment expands and evolves. For a deeper look into the market dynamics and long-term projections, see the external resource linked at the end of this chapter. Within the realm of practice, one may also consider how current research on technology integration in OT aligns with or challenges existing workflows, guidelines, and reimbursement structures. A practical takeaway for clinicians is to start integrating wearable and AR/VR tools in a measured, patient-centered way, prioritizing devices that demonstrate clear clinical value, ease of use, and a reasonable path to home-based application. By embracing these innovations thoughtfully, occupational therapists can maintain the profession’s core commitment to enabling people to engage with their daily lives more fully, while extending support beyond the clinic walls.
To situate these developments within the broader field, it is helpful to consider the research and discourse that frame this evolution. The convergence of smart devices, wearable sensors, and adaptive software is not an isolated trend but part of a wider shift toward data-informed, home-centered rehabilitation. Evidence synthesized in recent years underscores the effectiveness of motor learning principles when delivered through feedback-rich, interactive modalities. The emphasis on active participation, goal-directed practice, and contextualized tasks aligns closely with what patients value most: the ability to perform meaningful activities with confidence and safety. This alignment helps ensure that the adoption of new equipment supports, rather than distracts from, therapeutic aims. As this field advances, ongoing collaboration among clinicians, engineers, researchers, and patients will be essential to refine interfaces, improve usability, and expand the repertoire of activities that can be practiced meaningfully in real-world settings.
In this future-forward view, the role of the occupational therapy professional remains central. Technology acts as an amplifier of expertise, not a replacement for it. The therapist curates the selection of devices, interprets the data, translates information into actionable goals, and maintains the human-centered core of care. The patient’s lived experience—the everyday tasks that carry meaning, identity, and purpose—drives the choice of activities, the pacing of progress, and the interpretation of success. The equipment fosters a shared journey: the patient as the lead actor, the therapist as guide, and the tool as a reliable partner that records, reflects, and reinforces gains. As this trajectory unfolds, OT practice will increasingly balance the precision of analytics with the nuance of personhood, ensuring that advancement in therapy technology translates into tangible improvements in independence, quality of life, and the dignity of everyday living.
Readers may wish to explore further the broader implications for policy and practice as the market for durable medical equipment expands and evolves. For a deeper look into the market dynamics and long-term projections, see the external resource linked at the end of this chapter. Within the realm of practice, one may also consider how current research on technology integration in OT aligns with or challenges existing workflows, guidelines, and reimbursement structures. A practical takeaway for clinicians is to start integrating wearable and AR/VR tools in a measured, patient-centered way, prioritizing devices that demonstrate clear clinical value, ease of use, and a reasonable path to home-based application. By embracing these innovations thoughtfully, occupational therapists can maintain the profession’s core commitment to enabling people to engage with their daily lives more fully, while extending support beyond the clinic walls.
To situate these developments within the broader field, it is helpful to consider the research and discourse that frame this evolution. The convergence of smart devices, wearable sensors, and adaptive software is not an isolated trend but part of a wider shift toward data-informed, home-centered rehabilitation. Evidence synthesized in recent years underscores the effectiveness of motor learning principles when delivered through feedback-rich, interactive modalities. The emphasis on active participation, goal-directed practice, and contextualized tasks aligns closely with what patients value most: the ability to perform meaningful activities with confidence and safety. This alignment helps ensure that the adoption of new equipment supports, rather than distracts from, therapeutic aims. As this field advances, ongoing collaboration among clinicians, engineers, researchers, and patients will be essential to refine interfaces, improve usability, and expand the repertoire of activities that can be practiced meaningfully in real-world settings.
In sum, the future of OT equipment rests on the seamless integration of smart wearables, immersive realities, and AI-driven analytics, all deployed within a supportive, patient-centered framework. The next generation of devices will be designed to travel with patients, adapt to changing needs, and deliver feedback that is timely, relevant, and motivating. They will support ongoing practice at home, in the community, and across the continuum of care, while preserving the essential human elements of empathy, collaboration, and clinical judgment. As this trajectory unfolds, therapists will be empowered to tailor interventions with unprecedented precision, helping each person translate small, consistent gains into lasting independence. For readers interested in how these technologies intersect with broader market dynamics and policy considerations, the external resource at the end of this chapter provides a rigorous framework for understanding the evolving landscape of durable medical equipment and its implications for occupational therapy practice.
Final thoughts
Occupational therapy plays a crucial role in helping individuals regain their independence after injury or illness, and the equipment used in this field is pivotal to effective rehabilitation. Essential tools like grip strengtheners and adaptive utensils, along with innovative technologies, significantly improve outcomes and provide new avenues for independence. As the industry evolves, staying informed about future trends will ensure that therapy practices remain effective and relevant. Thus, investing in the right equipment is not just beneficial; it offers the promise of empowering lives.