Occupational therapy (OT) items play a pivotal role in the rehabilitation process, supporting individuals in enhancing their ability to perform daily activities. For business owners in the healthcare sector, understanding the importance of these tools is crucial, as they directly impact patient recovery and independence. This article explores the significance of occupational therapy items in rehabilitation, outlines the various types and their applications, and examines the profound impact these tools have on patient outcomes. By delving into each aspect, we aim to provide a holistic understanding of how OT items can be effectively integrated into rehabilitation practices, ultimately benefiting both patients and practitioners alike.
null
null
Tools That Build Everyday Confidence: An Integrated View of Occupational Therapy Items and Their Role in Independence
In the practice of occupational therapy, the objects that fill clinics, rehabilitation centers, and home therapy spaces carry more meaning than their material forms. They are carefully chosen allies whose design, arrangement, and progression map a path from challenge to competence. The goal is not merely to exercise a muscle or test a skill; it is to translate therapeutic effort into everyday capability. When a person reaches for a tool that fits their hand, or engages with an activity that mirrors a real life task, the therapy becomes relevant, motivating, and durable. The variety of items used in OT underscores a simple truth: independence is built through repeated, meaningful experiences that are adapted to each client’s abilities, goals, and preferences. In this broad yet interconnected landscape, several categories of items stand out for their versatility, their alignment with core occupational outcomes, and their capacity to be tailored to individual journeys toward meaningful occupations such as dressing, feeding, writing, and community participation.
One broad category centers on sensory integration tools. These items are chosen for their ability to gently and predictably influence the nervous system, aiding regulation, attention, and readiness for activity. In pediatric settings especially, swinging structures and climbing apparatus provide vestibular input that supports balance, spatial awareness, and tolerance to movement. Textured materials, tactile toys, and weighted or adaptive textiles offer graded sensory stimulation that can calm or alert depending on the need. The therapist uses these tools not as ends in themselves but as means to prime the nervous system for task engagement. For a child who becomes overwhelmed by crowded environments, a sensory activity can lower anxiety enough to approach a writing task or a dressing activity with less distraction. The same idea translates into adult contexts as well, where sensory-based strategies can aid mood regulation and focus in the face of fatigue or cognitive load. The journey here is not about pushing a single skill but about shaping the sensory state that makes skill practice possible.
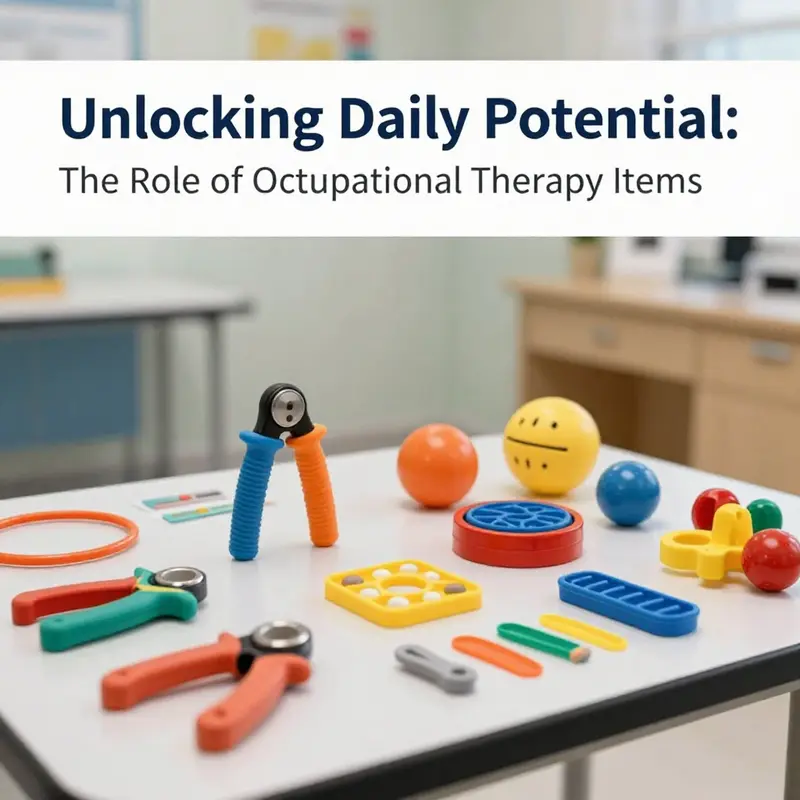
When sensory input is balanced with other demands, therapists turn to fine motor and dexterity aids. The objective is precise and purposeful movement that supports daily tasks such as buttoning a shirt, gripping utensils, turning a page, or manipulating a zipper. Tools like putty or textured clay enable repetitive hand strengthening and finger isolation without excessive strain. Therapy balls, small manipulatives, and finger exercisers provide graded resistance, allowing gradual progression from easier to more challenging grips and releases. These items help rebuild the intricate coordination required for writing, drawing, and manipulating small fasteners. In addition, arts and crafts materials — beads, scissors, glue, and simple construction items — are not merely fun. They offer structured practice that blends sensory feedback with motor control and cognitive planning. The active engagement involved in selecting, sorting, and sequencing beads or gluing shapes promotes hand-eye coordination, bilateral coordination, and sustained attention in a context that feels purposeful and creative.
Adaptive equipment and activity-specific tools broaden the reach of therapy into real world tasks. These items simulate everyday movements in a safe, controlled way while maintaining the unpredictability of real life. Therapy gym equipment, in particular, is designed to bridge clinic and home environments. It supports functional practice with safety, enabling clients to perform dissociated or integrated movements that mirror daily activities. For instance, a therapy setup might guide someone through simulated kitchen tasks or dressing routines while providing feedback and resistance that increase gradually with competence. In addition, tools such as weighted blankets, fidget toys, and visual schedules support aspects of mental health, anxiety management, and executive functioning. A weighted blanket can offer comforting proprioceptive input, potentially reducing restlessness during tasks that require sustained attention. Fidget toys provide discreet avenues for self-regulation, particularly during transitions or problem solving. Visual schedules help individuals with ADHD or autism spectrum disorders organize sequences of activities, reducing cognitive load and improving the likelihood of independent participation in daily routines. Together, these items illustrate how OT expands beyond the physical to influence cognitive and emotional readiness, which is essential to true independence.
The way practitioners select and apply these items matters as much as the items themselves. This is where best practices and individualized treatment planning come into clear focus. The process begins with a comprehensive assessment of the client’s abilities, environment, and goals. The therapist identifies which items can illuminate strengths, reduce barriers, and provide a stepping stone toward meaningful tasks. From there, the items are arranged to create a meaningful sequence. A familiar kitchen task might be practiced first with light resistance and simplified equipment, then advanced as confidence grows. A dressing task could involve adapted fasteners or grips that match the person’s current hand function. Throughout this journey, the therapist remains attentive to safety, comfort, and the client’s preferences. The aim is to avoid a one size fits all approach; instead, the selection and progression of items are tightly aligned with the client’s everyday occupations and the values that matter most to them.
This approach to equipment selection naturally leads to considerations about how therapists stay current and how they please the eye and the hand with the right balance of challenge and accessibility. A thoughtful practitioner will consult guidelines from professional bodies and turn to practical resources on equipment selection, ensuring that each item serves a clear therapeutic purpose. In practice, this means not only choosing the right tool but also configuring it to accommodate any coexisting conditions such as arthritis, tremor, or sensory sensitivity. The person might need larger grips or softer textures, or perhaps a sequence design that minimizes fatigue while maximizing function. The ultimate measure of success is not the presence of a particular tool in a session but the client’s ability to use it as a vehicle to participate more fully in daily life. When a client can complete a daily task with less assistance, or when a child can transition more smoothly between activities at school or home, the therapy has moved closer to its core aim—functional independence in the real world.
As therapy unfolds, the conversation between client and therapist often expands to include the home environment and the broader community. Therapists increasingly acknowledge the value of home setup and community-based practice in promoting carryover. The items chosen for clinic sessions are then translated into home programs that typically require minimal equipment but high relevance. For example, a simple set of hand strengthening activities could be integrated into a kitchen routine, a craft project could be pursued in a dining room or classroom, and a visual schedule could be posted in a familiar hall or bedroom. The seamless transfer from clinic to home hinges on a mutual understanding of goals, a careful selection of adaptable tools, and ongoing communication between therapist, client, and family. In this light, OT items become a bridge rather than a barrier, linking the controlled environment of therapy with the dynamic, evolving demands of daily life.
In the broader landscape of occupational therapy, the careful choice of items is also informed by a multidisciplinary view of patient care. Therapists collaborate with educators, nurses, physicians, and caregivers to align equipment choices with overarching treatment plans and safety considerations. This collaboration ensures that the tools used in therapy do not exist in isolation but are chosen with an eye toward continuity of care, risk management, and the client’s overall well-being. As a result, the items in therapy rooms, gyms, and at home embody a philosophy of person-centered care that respects each client’s unique rhythm, pace, and preferences. The emphasis remains on real-world relevance, purposeful practice, and the durable gains that come from consistent, meaningful engagement with tools that are designed to adapt to changing needs.
To be practical and informed, therapists often consult resource collections that translate theory into actionable guidance. These resources emphasize how to assess the performance of gym equipment, how to select materials with appropriate resistance and texture, and how to structure therapy sessions so that equipment use remains safe, engaging, and effective. The emphasis on proper technique is crucial; even well-chosen items can pose risks if used without appropriate training or supervision. Therapists must model correct use, monitor for discomfort, and adjust intensity to prevent strain or injury. This careful, educated approach ensures that the items support progress rather than hinder it, and it helps protect the client from overexertion while nurturing resilience and competence in everyday activities.
Through this integrated lens, the value of OT items becomes evident. They are not gimmicks or generic tools; they are calibrated instruments that contribute to a client’s sense of mastery and control. They enable repeated practice in contexts that feel authentic and relevant. They offer sensory input, motor challenge, and cognitive structure in ways that align with each person’s functional goals. They can be scaled up or down, modified for right or left handed use, or adapted to accommodate a range of sensory and motor profiles. They invite clients to participate actively, to notice small improvements, and to celebrate incremental successes that accumulate over days, weeks, and months. In this way, the intimate relationship between person, task, and tool becomes a powerful engine for growth, independence, and quality of life.
For readers seeking further exploration of how equipment choices influence therapeutic outcomes, consider resources that discuss practical equipment selection and usage. A useful internal reference is found in the article on tools and equipment for occupational therapists, which provides guidance on selecting appropriate items and implementing them in a therapeutic plan. This resource helps practitioners translate clinical thinking into real world practice, ensuring that the tools used in therapy rooms truly support daily independence and meaningful participation. As you continue to explore the domain of OT items, remember that the core intent remains simple and profound: empower clients to engage in what matters most to them, with tools that respect their pace, preferences, and dignity.
External resource: For a broader understanding of gym equipment design, performance, and industry best practices, see https://www.therapeuticproducts.com/ot-gym-equipment-overview
Tools of Transformation: How Occupational Therapy Items Shape Participation and Independence
Occupational therapy items are often tucked away in drawers, benches, and cupboards, yet they are not mere utensils. They are dynamic agents that organize the rhythms of a person’s day, reshaping what is possible and what is meaningful. In the best IEPs, rehab plans, and clinic sessions, these items operate as the tangible interface between a person’s goals and their everyday environment. They invite action, provide the scaffolding for new skill acquisition, and create predictable pathways through challenges that once seemed insurmountable. Rather than presenting a fixed repertoire of exercises, occupational therapy items become conduits for participation, enabling people to re-enter the occupations that define their identities—from dressing and cooking to managing finances, engaging with friends, and pursuing leisure activities that sustain mental well-being. In this sense, the items themselves are not ends but means through which individuals negotiate the complex choreography of daily life. They help translate a patient’s goals into achievable tasks, and they do so across settings, from hospital rooms to home kitchens and community centers. The result is not simply improved performance on a test, but a felt shift in what the person can do, how they feel about doing it, and how often they choose to engage in meaningful activities. This alignment of capability and choice lies at the heart of occupational therapy’s impact on patient outcomes.
The ultimate aim of occupational therapy is participation in meaningful daily activities, a broad and person-centered outcome that extends beyond the walls of a clinic. It includes the capacity to engage in role-appropriate activities, to enjoy leisure, to participate in community life, and to manage the practicalities of everyday living with increasing independence. OT items are critical enablers of this aim because they convert therapeutic intent into actionable steps. A set of manipulatives can improve finger strength and dexterity, but more importantly, they grant a patient the ability to button a shirt, grip a mug securely, or turn a page in a book without fatigue. A pair of adaptable hand tools and supportive grips can transform kitchen tasks from frustrating hurdles into routine accomplishments. In every case, the item serves as an affordance—the perceived and actual facilitate of action—that helps the person move from limitation toward meaningful engagement. The relationship between item and activity is not static. It evolves with the person’s growing skill, changing health status, and shifting life roles. In therapy, this dynamic is a core design principle: items are selected and progressively adjusted to maintain alignment with authentic goals, daily contexts, and the patient’s evolving sense of mastery.
A crucial dimension of this dynamic involves the interplay between what a person wants to do and what the environment supports. The Canadian Occupational Performance Measure (COPM) and the Client-Oriented Scale of Improvement (COSI) are standard tools through which therapists capture this interplay. COPM centers on the client’s own perception of performance and satisfaction in self-identified occupations, inviting a narrative of change that begins in the patient’s living room and extends to broader life domains. COSI complements COPM by focusing on client-specific goals and the degree to which those goals are met, offering a concise, patient-led progress map that can be revisited across time. When OT items are chosen with these measures in mind, the therapist gains a reliable lens to translate a person’s lived experience into quantifiable progress. The result is a practice anchored in what matters most to the patient, rather than what is convenient to measure in a clinical test. This client-centered orientation is not an abstract ideal; it is a practical framework that guides equipment selection, progression, and the scope of home exercise programs.
The broader literature consistently reinforces this approach. Townsend and Polatajko (2013) argued that enhanced participation in occupations is a unique and critical outcome of OT, one that transcends mere remediation of impairment. Their perspective remains foundational for contemporary practice, emphasizing how engagement in meaningful tasks reflects the core purpose of occupational therapy. In modern research, this emphasis on participation has become more formalized through validated outcome measures, but it also remains grounded in the therapist’s clinical intuition about what constitutes meaningful activity for a particular client. The 2022 study by C. Hand further underlines this point by highlighting the utility and feasibility of patient-centered interventions. Hand’s work demonstrates that tailoring interventions to the individual’s goals—especially those related to everyday functioning—can produce measurable gains in participation and independence. The takeaway is straightforward: when therapists connect interventions to what clients actually want to do in daily life, patients report higher satisfaction and show more sustained improvements over time. The synthesis of these ideas suggests that OT items, when embedded in a client-centered goal framework, become catalysts for durable participation gains rather than quick fixes for isolated deficits.
To appreciate how items translate into outcomes, consider the spectrum of everyday tasks that people want to perform and the contexts in which they occur. Some tasks require precise fine motor control and coordination; others demand strength endurance or postural stability. Still others depend on cognitive planning, sequencing, and problem-solving under real-life pressure. OT items are selected to address these diverse demands in a way that remains faithful to the person’s goals and living situation. For a patient recovering from a hand injury, a variety of hand-held tools and manipulatives can diversify practice, incorporating pinch, grip, and opposition patterns that build strength while simulating real-world tasks. For a person managing arthritis, tools that facilitate safe grip, reduce joint strain, and promote ergonomic movement patterns can sustain participation in daily routines without exacerbating pain. For children and adolescents, smaller-scale tools that promote play, school participation, and social interaction can bridge therapy sessions with the classroom or playground. Across all populations, the aim remains the same: to convert therapeutic effort into a reliable capacity to perform meaningful activities with less effort, less pain, and more confidence.
The selection and use of OT items are most effective when they are anchored in a thorough activity analysis that considers the person, the task, and the environment. This analysis is not a one-off exercise but an ongoing diagnostic and design tool. It requires the therapist to observe, question, and adjust. The patient’s home environment might present constraints that a clinic cannot replicate: uneven surfaces, cluttered workspaces, or limited assistive space. A therapist might then introduce items that address these environmental barriers, such as adaptive devices to stabilize utensils during meals or grips that distribute pressure more evenly across the hand. The goal is not to force a patient to adapt to the device but to adapt the device to fit the patient’s daily life. When the device aligns with the person’s environment and the task’s demands, it fosters a sense of competence. This sense, in turn, reinforces motivation and adherence to home programs. The translation from clinic to home is the moment when the item earns its true value.
The practical implications of these ideas extend beyond rehabilitation centers into home therapy programs and community settings. OT items can be designed or selected to support transitions—returning to work, re-engaging with family routines, resuming self-care activities, or embracing leisure that had fallen by the wayside. The continuum from beginner to more advanced skills often mirrors a parallel continuum of item complexity and resistance. A therapist might begin with simple, low-demand tasks, gradually layering on more challenging materials, and testing the patient’s capacity to generalize skills to unstructured situations. The critical factor is that progression remains aligned with the client’s goals and daily life—progression that is validated by COPM scores, COSI outcomes, and the patient’s own account of improved participation. In practice, this means that an item’s value is measured not only by how many repetitions can be performed but by how effectively it supports the patient’s ability to engage, enjoy, and sustain activity across contexts.
One way clinicians operationalize this alignment is through the careful pairing of specific tasks with corresponding items that support them while also serving as therapeutic challenges. A grip-strength training set, for example, offers a spectrum of resistance and grip patterns that can be calibrated to an individual’s strength profile and activity priorities. Although the precise product names aren’t the focus here, the principle is clear: a multi-faceted toolkit can scaffold the gradual return to functional independence, enabling patients to practice precision grips for buttoning, sustained grip for carrying objects, and dynamic grips for opening jars or turning doorknobs. The versatility of such kits makes them suitable for both structured therapy sessions and informal, at-home practice, which in turn amplifies the likelihood of transfer from clinical gains to real-world independence. The broader value lies in how these items support repetition, variability, and meaningful practice—core elements that drive durable improvements in daily life.
A critical concern in this work is ensuring that outcome measures capture the full range of participation gains resulting from item-based interventions. Traditional impairment-focused metrics can miss the day-to-day improvements that matter most to patients. COPM and COSI address this gap by prioritizing patient-defined outcomes and by tracking changes that reflect real-life functioning rather than laboratory performance alone. When therapists document progress in COPM domains such as self-care, productivity, and leisure, they articulate a narrative that connects item use with concrete life improvements. This narrative is essential because it helps clinicians, patients, families, and payers understand the rationale for continued therapy and for the ongoing investment in adaptive equipment and home modifications. Moreover, COPM and COSI provide a shared language for interdisciplinary teams. When occupational therapists collaborate with physical therapists, speech-language pathologists, psychologists, and social workers, the patient’s goals can be reframed as a shared objective in which items act as the central tools that support cross-disciplinary participation in daily life. In this sense, items do not exist in isolation; they become focal points around which the patient’s ecosystem of care is organized.
Despite the emphasis on client-centered measurement, there is a need for practical guidance about item selection that can be generalized across settings without diluting individualization. The literature supports this balance. Clinicians can use general frameworks to screen items for safety, usability, adaptability, and cultural relevance, while still calibrating selection to each patient’s specific goals. A notable advantage of incorporating client-centered measures early in the process is that it helps identify potential barriers to participation before they become entrenched. For instance, a patient who values independent dressing may be hindered not by a lack of strength alone, but by a lack of energy, fatigue, or poor sequencing of steps. An OT item that supports grip and dexterity might be paired with a timer, a simplified sequence, or a cueing strategy to ensure consistent engagement. In this way, items become part of a holistic plan that addresses physical capacity, cognitive organization, and emotional readiness—all of which contribute to the patient’s sense of agency and satisfaction with therapy.
The role of technology and innovation in this domain is meaningful but should be understood as additive rather than revolutionary. Technology can augment the functional reach of OT items through enhanced feedback, better ergonomic design, or data capture that clarifies progress. Yet the core insight remains that success hinges on aligning tools with what patients value and where they live. The most effective practitioners continuously ask themselves: What matters to this patient in this season of life? What barriers are most salient in the home or community? What would a sustainable routine look like, with the fewest possible frictions that might derail progress? And how can the equipment in hand be optimized to reduce those frictions while promoting growth? The answers to these questions often determine the difference between a therapy plan that feels like a collection of exercises and a living, adaptive program that supports ongoing participation.
In closing, the evidence from contemporary OT outcomes research emphasizes that meaningful gains in daily life emerge when therapy items are thoughtfully integrated into client-centered goals. The COPM and COSI frameworks help therapists capture and communicate these gains, while the broader theoretical contributions of Townsend and Polatajko remind us that participation in meaningful occupations is the ultimate indicator of success. Hand’s 2022 work reinforces the practical value of tailoring interventions to individual needs, showing that personalized approaches yield tangible improvements in participation and independence. Together, these strands offer a coherent view of how items—when chosen with care, applied with intention, and evaluated with sensitive measures—become potent levers for change. They transform therapy from a sequence of tasks into a collaborative journey toward reclaimed living. For clinicians who seek a pragmatic route to optimize outcomes, a guiding principle emerges: select items not only for their mechanical properties but for their capacity to enable the patient’s chosen occupations, in the contexts that matter most to them, at a pace that respects their life, energy, and dignity. In this sense, the right OT item is not merely a tool; it is a partner in a shared pursuit of independence, participation, and quality of life. To further explore the practical resources that support this approach, clinicians can consult comprehensive guides on tools and equipment for occupational therapists, which offer structured insights into selecting, adapting, and integrating devices within patient-centered practice. Tools and equipment for occupational therapists. For a detailed discussion of measurement tools and methods in occupational therapy, practitioners may refer to peer-reviewed syntheses and guidelines that illuminate how to design, implement, and interpret outcome measures across diverse populations. A foundational resource in this regard is the article on measuring the outcome of occupational therapy, which reviews practical tools and frameworks for evaluating progress over time. See https://www.ncbi.nlm.nih.nih.gov/pmc/articles/PMC9587467/ for an in-depth exploration of these approaches.
Final thoughts
As healthcare providers increasingly recognize the importance of occupational therapy items, their role in enhancing rehabilitation outcomes becomes clear. These tools not only aid in the recovery process but also empower patients towards achieving greater independence in their daily lives. For business owners, investing in quality OT items can enhance service offerings and ultimately improve patient satisfaction and health outcomes. By fostering an environment that prioritizes effective therapeutics, you can stand out in the competitive healthcare landscape while making a meaningful difference in the recovery journey of your clients.