Understanding the differences between physical therapy (PT) and occupational therapy (OT) is crucial for business owners in healthcare-related fields. Both disciplines aim to improve patients’ functional abilities, yet they do so through distinct goals, methods, and applications. In this article, we will delve into these differences, exploring the primary objectives of each therapy, their unique techniques, and the types of conditions they address. Additionally, we will analyze the importance of collaboration between PTs and OTs, highlighting how an integrated approach can enhance care quality and patient outcomes. As we navigate these chapters, business owners will gain insights essential for making informed decisions about staffing, service offerings, and patient management.
Two Paths to Recovery: How Physical Therapy and Occupational Therapy Distinguish Yet Converge in Reclaiming Everyday Life
Physical therapy focuses on movement as the core path to health, using exercises, manual techniques, and modalities to restore range of motion, strength, and endurance. Occupational therapy centers on daily life and meaningful participation, tailoring strategies to help self care, work, and home tasks through adaptive equipment, environmental changes, and cognitive strategies. Both aim to reduce pain, prevent disability, and improve independence, but PT orients toward movement, while OT emphasizes functional engagement in real contexts. In practice they collaborate: PT builds the capacity to move safely, OT translates that capacity into reliable routines and tasks, and together they align goals with the person’s daily life. Education and rehab planning address function in home, work, and community, with regular reassessment and adjustment. Training pathways differ: PT often requires Doctor of Physical Therapy or similar advanced training; OT typically involves Master of Occupational Therapy or equivalent. The ultimate aim is a person-centered recovery where improved movement and improved ability to perform daily activities reinforce each other, enabling a fuller, more durable independence.
Clarifying the Distinct Goals of Physical Therapy and Occupational Therapy
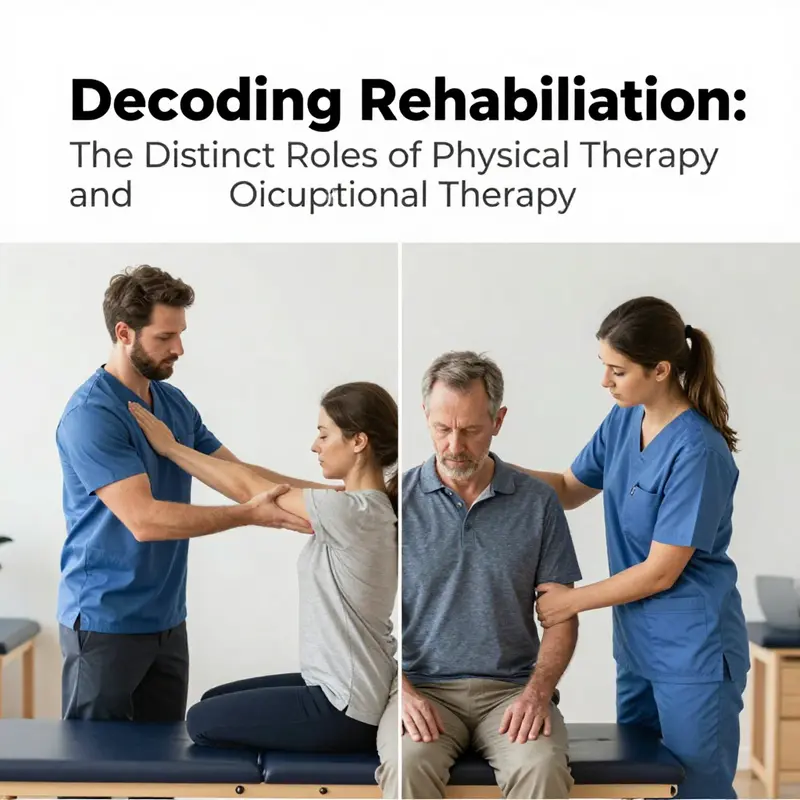
In rehabilitation, two professions often share a patient’s journey toward greater independence, yet they chart different courses and answer different questions. Physical therapy (PT) asks: How can we restore movement, strength, and physical function so that a person can move with less pain and more reliability? Occupational therapy (OT) asks: How can a person participate in daily life—self-care, work, and meaningful activities—despite physical or cognitive challenges? Reading these questions side by side helps illuminate not only what each discipline prioritizes, but also how their combined efforts create a more complete map back to everyday life.\n\nTo understand the goals of PT, imagine a person recovering from knee surgery. The earliest focus is on the mechanics of the leg—how the knee bends, how the muscles support the joint, and how the person can walk again without limping. Physical therapists guide patients through exercises designed to build strength, improve flexibility, and restore balance and endurance. They assess gait patterns, work on range of motion, and use manual therapy to ease stiffness. Therapeutic modalities such as heat or cold, ultrasound, or electrical stimulation may be employed to reduce pain and promote healing. Importantly, the aim is not only to return someone to walking but to restore confidence in movement across various tasks, from climbing stairs to standing from a chair without assistance. Alongside physical gains, PT emphasizes education about body mechanics. Patients learn safer ways to move, lift, and position their bodies to prevent re-injury once they return to daily routines.\n\nIn contrast, OT centers on the tasks a person performs every day and in the broader sense of what those tasks mean within a person’s life. Consider someone who has experienced a stroke and now faces challenges with dressing, cooking, or managing finances. An occupational therapist would assess how cognitive processing, sensory perception, fine motor skills, and motor precision affect these activities. The OT plan may include practicing dressing with one hand, using adaptive equipment, or reorganizing the home environment to reduce hazards. It also often addresses cognitive and perceptual components—memory strategies, problem-solving within a kitchen, or visual-spatial awareness needed to navigate a cluttered room. The objective is practical: to enable the person to engage in self-care, productive tasks, and leisure activities with safety and independence. This focus acknowledges that people are defined by how they live, not solely by how well they move in a clinic setting.\n\nAlthough PT and OT pursue different endpoints, their work is deeply interwoven. A patient recovering from a hip fracture may benefit from PT to regain leg strength and walking ability while an OT works on buttoning a shirt, preparing a simple meal, or managing medication schedules. In many rehabilitation settings, the two disciplines collaborate within a coordinated care plan that treats the whole person. One therapist’s progress in range of motion can create new possibilities for the other to address daily tasks. This collaboration ensures that gains in movement translate into real-life improvements in independence, safety, and confidence. The synergy becomes especially evident when a patient faces both physical and cognitive or sensory challenges. In such cases, PT may focus on restoring movement, while OT crafts environmental adaptations and compensatory strategies that make those movements meaningful in daily life.\n\nThe distinct goals of PT and OT also reflect their broader professional identities. PT speaks in the language of physical function. Its practitioners are tasked with enabling people to move with less pain, to perform tasks they could not do before, and to prevent disability through targeted exercise, manual techniques, and evidence-based interventions. OT speaks in terms of participation and role fulfillment. Its practitioners are charged with helping individuals reclaim their identities—whether as a patient who can dress independently, a parent who can prepare meals, or a worker who can return to the job with adapted routines. These identities matter because the sense of competence and purpose that comes from engaging in meaningful activities is a powerful driver of overall well-being and long-term adherence to therapy.\n\nWhen clinicians articulate these goals to patients and families, the message is practical and hopeful. PT outlines a path to movement—how to regain strength, how to reduce pain, how to walk securely, and how to protect joints during activity. OT translates that path into everyday meaning—how to push a chair to the table safely, how to organize a kitchen for one-handed cooking, how to manage morning routines with fewer frustrations. The ultimate aim is not merely rehabilitation in a clinical sense, but rehabilitation that returns people to their chosen roles and passions. In this sense, the two professions are not competitors but complementary partners in constructing a life that aligns with a person’s values and priorities.\n\nA common thread through both disciplines is patient-centeredness. Therapists begin by listening—what matters to the patient, what brings satisfaction, what fears exist about re-injury or dependence. From there, they tailor plans that respect a person’s priorities and living environment. For PT, that might mean prioritizing a safe ambulation plan for someone who uses a walking aid in daily life. For OT, it might involve designing a home modification plan or identifying assistive devices that enable independent self-care. The shared emphasis on education is crucial. Patients learn not only exercises or tasks but the reasons behind them, which strengthens motivation and facilitates long-term maintenance beyond the clinic walls.\n\nThese goals are not abstract ideals; they translate into concrete milestones that families and care teams can observe. A PT milestone might be achieving a pain-free step on uneven ground, or demonstrating improved squat mechanics that reduce knee strain during daily tasks. An OT milestone could be completing a morning routine without verbal prompts, managing self-care after a sensory overload, or entering a kitchen with adaptive tools and no fear of slipping. When milestones are framed in terms of real life—getting to work on time, preparing a healthy meal for a loved one, or dressing independently—the therapy becomes a lived part of the person’s story rather than a sequence of clinic sessions.\n\nIn clinical practice, this alignment of goals facilitates a holistic approach to recovery. PT and OT teams often share assessment data, discuss progress in movement and function, and adjust plans to ensure that improvements in one domain support gains in another. For patients facing complex conditions, such as post-stroke rehabilitation or after major orthopedic surgery, the collaboration becomes essential to achieving outcomes that are sustainable and meaningful. The patient’s home—its layout, lighting, and safety features—may become a central part of the therapy plan, guiding decisions about both movement training and environmental adaptations. By integrating movement restoration with functional participation, PT and OT together help people reclaim the daily rhythms that give life structure and joy.\n\nFor readers seeking a concise distinction, one can summarize the difference as a matter of emphasis: PT is primarily about movement and physical capability, while OT is about performing and engaging in life’s activities within a person’s environment. Yet this distinction sits atop a shared commitment to the person-centered, evidence-based improvement of health and quality of life. If you want to explore how these goals align in practical terms, you can read more about the nuance between the two fields in a focused discussion here: difference between physical therapy and occupational therapy.\n\nThe NHS offers a clear perspective from a UK lens, reinforcing that physical therapy and occupational therapy, while distinct, are often part of a unified rehabilitation journey designed to maximize independence and safety. The guidance emphasizes how PT targets movement and function, while OT emphasizes independence in daily living and participation in meaningful activities. Together, these paths create a comprehensive framework that supports a person’s return to normal life after injury or illness. As patients, families, and clinicians navigate a recovery plan, recognizing the specific goals of each discipline helps set realistic expectations, fosters collaboration, and keeps the focus on the outcomes that matter most in daily living. For those seeking a reputable overview from a broader healthcare system, consider the NHS resource linked below as a supportive reference point for understanding how PT and OT operate within a multidisciplinary team.\n\nExternal resource: https://www.nhs.uk/conditions/physical-therapy/
Moving Toward Independence: Distinctions and Shared Mission of Physical Therapy and Occupational Therapy
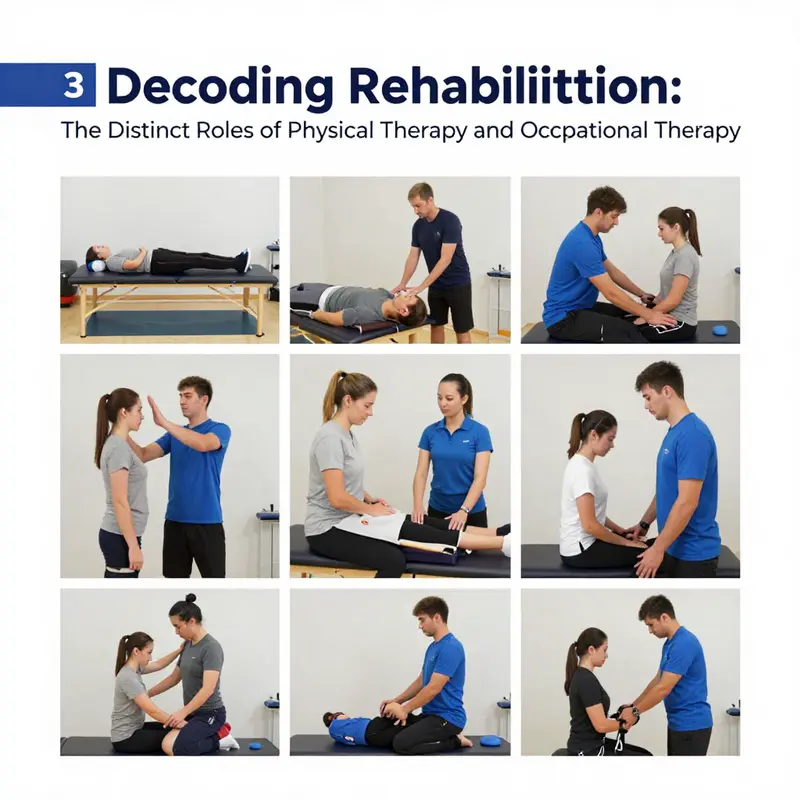
Physical therapy and occupational therapy are allied disciplines in rehabilitation, each answering different questions about daily life. They share a common goal: helping people regain function and participate more fully in everyday activities. They approach this goal from different angles. The physical therapist focuses on movement, strength, endurance, and the body’s ability to function during basic tasks. They assess joints, muscles, nerves, and gait, and design exercises to restore motion, build strength, and reduce pain. Manual therapy and modalities may accompany exercises to support healing. The objective is to restore physical capacity so the person can perform meaningful activities again, such as walking stairs or returning to a sport.
Occupational therapy is centered on daily tasks and roles. It asks how to adapt home, work, and leisure so a person can participate meaningfully. An OT looks at how tasks are performed, what environmental barriers exist, and what tools or strategies can help. They may train self care like dressing and bathing, or support activities like cooking and managing medications. They also address cognitive, sensory, or emotional challenges that affect daily function. The goal is not simply to move a limb, but to enable independence in the routines that matter most to the person.
In practice, PT and OT teams coordinate to tailor plans to each patient. A hip replacement may require PT to restore mobility and balance, while OT ensures safe dressing, bathing, and home management. A stroke rehab plan might blend OT for daily activities and PT for mobility and endurance. The two paths are complementary, not competing, and the patient benefits from a seamless partnership that respects the person’s goals, home environment, and support system.
Because independence is personal, the exact mix of PT and OT depends on the patient. Clinicians use objective measures and patient goals to track progress and adjust care. The joint approach helps people regain not just movement but confidence to participate in life with less pain and more choice.
Readers seeking further context can consult reliable resources that place PT and OT in a broader rehabilitation landscape. The key message remains: movement and daily activity are connected, and coordinated therapy supports a person’s happiest possible life.
null

null
null
null
Final thoughts
In conclusion, recognizing the distinction between physical therapy and occupational therapy is vital for effective patient care and informed business practices. While both therapies aim to improve patients’ functional abilities, their focus, methodologies, and treatment goals differ significantly. By fostering collaboration between PTs and OTs, healthcare providers can create a more comprehensive approach to rehabilitation that enhances patient outcomes and optimizes service delivery. As business owners in healthcare, understanding these nuances enables better staffing decisions and service offerings, ultimately contributing to a thriving practice focused on patient well-being.