Occupational therapy (OT) plays a crucial role in improving individual independence and quality of life through targeted interventions. From the developmental hurdles faced by children to the rehabilitation processes of adults, the expertise of occupational therapists spans various demographics and conditions. This article delves into three primary groups that OTs serve: children with developmental disorders, adults recovering from injuries, and older adults dealing with aging issues. Each chapter provides insight on how OTs assist these populations in achieving their personal and occupational goals, highlighting the diverse applications of OT in fostering engagement and enhancing functionality.
Nurturing Everyday Potential: How Occupational Therapists Support Children with Developmental Disorders
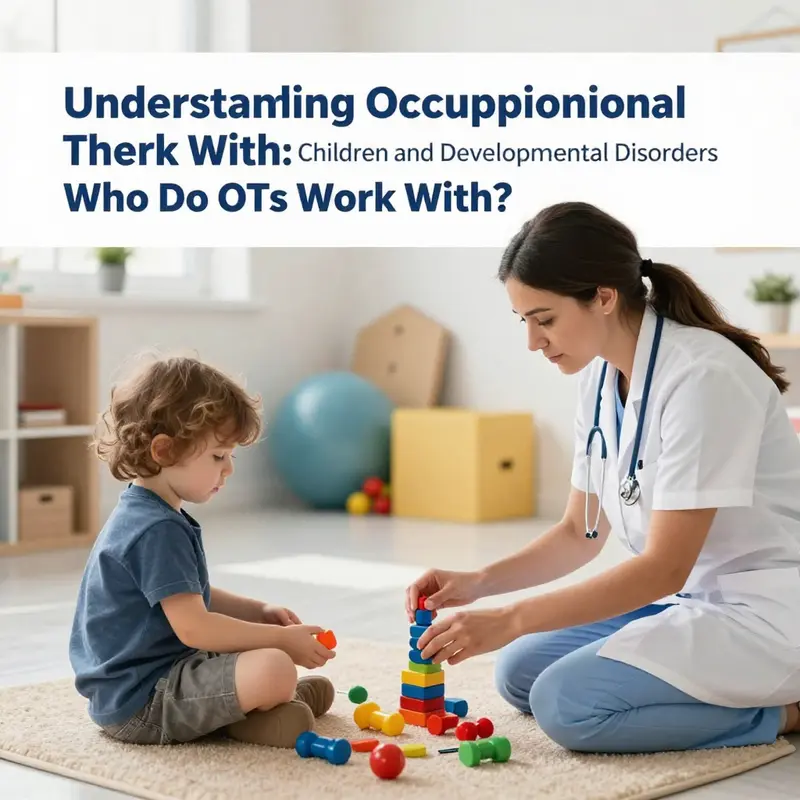
Every child brings a distinct rhythm of movement, thought, and engagement to daily life. When a developmental disorder touches that rhythm, the challenge is not simply a deficit to fix but a landscape to navigate with care, curiosity, and practical strategies. Occupational therapists, in partnership with families, educators, and healthcare teammates, stand beside children to translate the ordinary acts of living into accessible, meaningful participation. The phrase daily occupations may sound abstract, yet it is at the heart of what OTs do. They help children perform self care, participate in school routines, engage in play, and connect with peers in ways that respect each child s pace, preferences, and strengths. In this sense, the work is not just about improving fine motor skills or sensory responses in isolation. It is about weaving these skill gains into a functional tapestry that supports confidence, safety, and joy across the environments where a child grows, learns, and belongs.
When we center the child within developmental disorders such as autism spectrum disorder, ADHD, cerebral palsy, Down syndrome, sensory processing disorder, and various learning disabilities, a common thread emerges: each condition presents a unique constellation of challenges that can affect how a child moves, expresses emotion, processes sensory information, and organizes tasks. Yet across this diversity, the objective remains consistent and deeply practical. OT aims to empower the child to participate more fully in everyday life—at home, in school, during play, and in communities. This emphasis on participation reflects a fundamental shift from a deficit focus to a strengths-based, activity-centered approach. It invites families to imagine possibilities that align with the child s authentic interests and the family s routines, values, and aspirations, transforming what might feel overwhelming into a sequence of achievable steps.
To appreciate how OTs work with children, it helps to start from assessment. An OT begins by observing the child in natural settings—home, classroom, playground—watching how tasks unfold and where friction appears. They gather input from parents, teachers, and caregivers about what everyday activities look like, what is most meaningful to the child, and where the child struggles or shines. This information guides a holistic evaluation that considers multiple domains: fine motor control, the integration of visual information with motor planning, coordination of large and small movements, self-care abilities such as dressing and eating, and emotional regulation during tasks that can be stressful or overstimulating. The assessment is not a single test but a collaborative, iterative process that honors the child s changing needs across different contexts. It is also deeply informed by the family and the classroom setting, recognizing that occupational therapy is most effective when it aligns with the routines already shaping the child s days.
In autism focused care, for instance, the OT often addresses a blend of communication, social interaction, sensory processing, and adaptive play. The aim is not to normalize every behavior but to expand the child s capacity to participate in socially meaningful ways that feel safe and engaging. Structured play activities, visual schedules, and predictable routines can create a reliable framework that reduces anxiety and builds social reciprocity. Sensory strategies, such as a calming corner, sensory-friendly transitions, or tools that support self-regulation, help the child modulate arousal so that learning and interaction become possible rather than overwhelming. The teaching moments are embedded in play and everyday activities, ensuring the child experiences progress within moments of genuine interest and enjoyment. For families and clinicians seeking evidence based strategies, there are many resources exploring how OT approaches autism through specific interventions and tailored supports, including dedicated explorations of sensory processing, communication, and play.
The same careful orchestration of assessment and intervention appears across other developmental profiles. In kids with ADHD, the focus often shifts toward organization, sustained attention, and task planning. An OT might help break large tasks into manageable steps, teach consistent routines for arrival at school, lunch, and transitions, and modify the environment to reduce distractions. Tools such as visual checklists, color coded systems, and structured activity timers can support the child as they build independence in classroom tasks, self care, and after school routines. The objective is not to suppress energy but to channel it into productive, meaningful engagement that enhances the child s sense of competence. In cerebral palsy or Down syndrome, therapists work on foundational skills such as fine motor control, gross motor coordination, and self care while also addressing participation in school and community settings. The approach integrates assistive devices and adaptive equipment when appropriate, balancing the child s comfort, mobility, and autonomy with the demands of daily life. These examples illustrate a common thread: therapy is most effective when it respects the child s pace, honors family priorities, and remains flexible enough to adjust as the child grows.
A core feature of pediatric OT is activity analysis—the process of breaking down tasks into components to identify where a child experiences difficulty and where adjustments can yield meaningful participation. For a child who struggles with handwriting, the OT might examine grip strength, finger isolation, wrist stability, visual motor integration, and the cognitive planning required to form letters. The solution may involve a range of strategies: hand strengthening activities, scissors and craft tasks to refine precision, or ergonomic supports and alternative writing tools to reduce fatigue. In some cases, the intervention stresses posture and seating alignment, recognizing that efficient movement begins with a supportive position. In others, the emphasis rests on sensory modulation, teaching the child to recognize internal cues of overwhelm and to use strategies that restore focus and calm. Each plan is crafted with input from the family and educators, ensuring the child can transfer gains from clinic sessions to real world settings. This transfer is the heart of occupational therapy, turning isolated skills into enduring participation.
The foray into sensory processing issues reveals another layer of the child s daily life. Many developmental disorders intersect with sensory differences, where a child may be overresponsive to sounds or textures or, conversely, underresponsive to sensory cues. The OT responds with a structured approach that blends predictability, sensory input, and meaningful activities. A routine might incorporate sensory friendly activities before a challenging task, providing the child with a steady sensory diet that supports attention and engagement. Adaptive tools such as weighted blankets for calming, fidget devices for focused work, and tactile supports for fine motor tasks can be gently integrated into home and school routines. The aim is to help the child feel in control of sensory input rather than overwhelmed by it, so that daily tasks like dressing, eating, or participating in class become less anxiety provoking and more rewarding. In this framework, the child s environment is not a barrier but a collaborator, with schedules, materials, and spaces arranged to support successful participation.
The impact of occupational therapy extends beyond the individual child and ripples into family life, school culture, and community belonging. Parents gain practical skills to reinforce therapy goals at home, from consistent bedtime routines to step by step task guidance that reduces power struggles and promotes autonomy. Teachers learn ways to adapt classroom activities to accommodate diverse needs, such as offering visual supports, adjusting expectations for task duration, and facilitating social interactions that feel safe and inviting. The interdisciplinary team becomes stronger when each member understands the child s everyday realities and works toward common participation goals. Occupational therapists often collaborate with physicians, physical therapists, speech language pathologists, social workers, and educators to coordinate care plans. This teamwork ensures that goals are aligned across settings and that progress is sustained when the child transitions between home, school, and community environments.
For families seeking concrete examples of how therapy unfolds in daily life, imagine a morning routine for a child with a developmental disorder who is transitioning to school life. The OT might start by examining dressing skills, selecting clothes that are comfortable and easy to manage, and introducing a visual checklist that guides the steps from waking to leaving the door. The same child would then engage in a school day where tasks such as handwriting, cutting shapes, or organizing a locker are supported by adaptive strategies, careful seating, and a schedule that predicts transitions. The child learns to monitor emotions during these activities, recognizing signals of frustration before they escalate and using coping techniques learned in therapy. In this fluid flow of activities, progress is not a single event but a pattern of improved participation that grows with time, practice, and supportive relationships. The child gains competence not simply in completing tasks but in choosing activities, setting goals with the help of adults, and experiencing a sense of ownership over daily life.
When we consider the landscape of developmental disorders across childhood, it becomes clear that the OT s role is not limited to remediation of isolated skills. It is a commitment to creating a world in which a child can belong in the settings that matter most. A classroom is not just a place to learn letters and numbers; it is a social and emotional environment where the child s contributions are valued. A home is not merely a place to rest after school; it is a site for practicing independence and building family routines that reduce stress and increase predictability. In every context, OT practitioners frame interventions as practical, personalized, and feasible. They help families design small, achievable steps that accumulate into lasting change, respecting cultural values, family dynamics, and the child s evolving interests.
To support ongoing growth, OTs frequently use visual supports, task simplification strategies, and environmental modifications that enable efficient participation without demanding perfection. Visual schedules, for example, provide predictable sequences that ease transitions and reduce anxiety. Task breakdown helps children tackle complex activities by focusing on one component at a time. Environmental modifications might include arranging a desk space to reduce clutter or introducing seating options that support postural stability during tasks. These adjustments are not merely accommodations but enabling strategies that empower the child to participate with increasing independence and confidence. The OT s work, then, becomes a conversation about accessibility and inclusion: how can the world be shaped so that a child with developmental differences can join in, contribute, and feel successful in everyday life?
The journey of therapy is a collaborative narrative that evolves with the child. A core principle is fidelity to the child s voice—the willingness to listen to what the child enjoys, dislikes, fears, and desires. When families are invited to co create intervention plans, the therapy feels less like instruction and more like shared exploration. This shared exploration often uncovers the child s intrinsic motivations, whether that is a passion for building, drawing, or arranging objects into meaningful patterns. When therapy aligns with these interests, engagement deepens, practice becomes enjoyable, and the child s goals take on deeper significance. The result is not only skill development but also an enhanced sense of self efficacy: the belief that one can influence one s own life through purposeful action.
The reach of occupational therapy into mental health areas also intersects with developmental disorders. Many children experience anxiety, mood shifts, or difficulties regulating emotions during a busy school day or during transitions. OT interventions may support these emotional regulation processes through strategies that are concrete and transferable. For instance, a child might learn a step by step approach to calming during a stressful moment, choose a preferred coping tool, and practice these tools in a variety of settings. By strengthening self regulation, OT helps the child participate more fully in social play, classroom learning, and after school activities. This holistic perspective is consistent with the broader aim of pediatric OT: to help the child feel competent, connected, and capable of pursuing a meaningful life.
In sum, the work of an occupational therapist with children who have developmental disorders is about translating the complexity of a child s experiences into practical steps toward greater participation. It merges deep observation with evidence based practice, blending sensory processing strategies, motor skill development, and social learning in a way that feels natural to the child. It also honors family knowledge, cultural context, and school realities, recognizing that progress happens where care meets everyday life. The child is at the center, but the child is not alone. A network of caregivers, educators, clinicians, and peers joins in to support growth, celebrate small victories, and problem solve together when barriers arise. Through this collaborative, child centered approach, occupational therapy nurtures everyday potential, turning daily routines into opportunities for achievement, belonging, and joy. For families exploring more on autism specific approaches, see the resource dedicated to how OT addresses autism, an example of the kind of targeted strategies that can be integrated into daily life. occupational therapy for autism.
As part of a larger system of care, pediatric occupational therapy also emphasizes the significance of school based practice. The school setting is a central arena where children spend a substantial portion of their day, and where functional participation translates into academic success and social inclusion. OTs in schools collaborate with teachers to adapt lessons, organize classroom materials, and design hands on activities that align with learning objectives while honoring the child s processing style. They might help restructure a science project so it accommodates visual learning strengths, reorganize a desk to reduce visual clutter, or introduce adaptive handwriting tools that preserve legibility without causing fatigue. This kind of collaboration underscores the interconnectedness of therapy with education, family life, and community participation. The goal remains stable: reduce barriers, maximize participation, and cultivate a sense of autonomy that supports long term growth.
The pathway forward for a child with a developmental disorder is not a fixed route but a dynamic process of adjustment and growth. Occupational therapy provides a flexible framework that can adapt to a child s changing needs as they progress through infancy, toddler years, school age, and into adolescence. It remains anchored in practical outcomes—better self care, more confident participation in class, smoother transitions, and richer social play experiences. It also keeps faith with the child s personal interests and strengths, ensuring that therapy supports a life that feels meaningful rather than merely more efficient. In the end, the child s everyday life becomes less about meeting a standard and more about discovering a sense of belonging and capability within the world they inhabit.
For families and professionals seeking a broader professional lens on this work, the following resource offers a comprehensive overview of how pediatric occupational therapy supports children and youth across diverse developmental profiles. External link: https://www.aota.org/About-Occupational-Therapy/Children-and-Youth
Rebuilding Independence: How Occupational Therapists Guide Adults Through Rehabilitation and Everyday Recovery
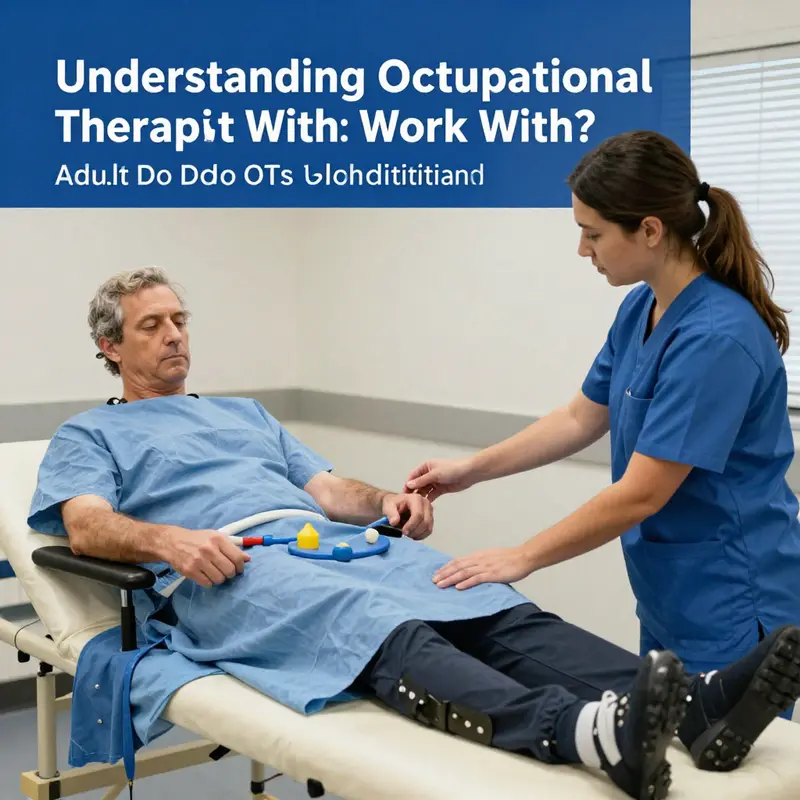
Across the arc of adulthood, rehabilitation is not a single event but a path that weaves together goals, routines, and the daily tasks that give life meaning. When we ask who an occupational therapist works with, the answer grows from a simple premise: OTs partner with adults who are navigating changes in ability, circumstance, or health status. They stand beside people recovering from injuries or surgeries, coping with chronic illnesses, adapting to neurological changes, or managing the demands of chronic conditions that affect energy, movement, and mood. The work is not only about regaining strength or mobility; it is about restoring participation—how a person sits at the table, dresses for work, prepares a meal for a family, or returns to a job they value. It is about aligning what a person wants to do with what they can do, given the realities of their body, their environment, and the roles they inhabit.
In rehabilitation, adults arrive with a mosaic of needs, each piece shaped by injury, disease, age, and life context. Some have emerged from the upheaval of a stroke, a spinal injury, or a hand surgery. Others live with chronic conditions such as obesity, diabetes, arthritis, or heart disease that slowly reshape daily patterns and purpose. Still others carry the invisible burdens of mental health challenges or cognitive changes that alter how one plans, initiates, and completes tasks. A common thread through all these scenarios is the central aim: to restore autonomy and to strengthen the capacity to participate in meaningful activities, whether that meaning is found in work, family life, hobbies, or self-care routines. This is not a one-size-fits-all process. It unfolds through a careful, collaborative exploration of a person’s priorities, the skills they bring to everyday life, and the environments in which they live.
The assessment that sets rehabilitation in motion is both practical and deeply person-centered. An occupational therapist begins by observing how a person currently performs everyday tasks. They examine not only the physical movements required but the cognitive planning, the sensory processing, and the emotional readiness involved in each activity. They listen for what matters most to the client—whether that is returning to a beloved hobby, staying independent at home, or resuming responsibilities at work. This listening is paired with standardized measures of function and skill. The clinician notes how a person uses energy during a task, how they sequence steps, how they adapt when a tool is not available, and where fear or frustration interrupts progress. The goal is to identify barriers and leverage strengths, to map out a pathway that honors the person’s values while accommodating the realities of their body and life. For adults facing obesity or other lifestyle-linked conditions, the assessment may extend beyond the screen of a single diagnosis. It becomes an inquiry into daily routines, dietary patterns, sleep quality, social support, and environmental demands—factors that together shape long-term health outcomes and the capacity to engage in daily life.
From assessment springs intervention that is both practical and aspirational. An OT designs activities and modifies environments to enable safer, more efficient performance of daily tasks. They might teach energy conservation strategies to someone recovering from a serious illness, helping them balance rest and activity so fatigue does not derail progress. They may introduce adaptive equipment or simple ergonomic adjustments at home or in the workplace to reduce strain and risk of injury. The interventions are chosen in close partnership with the client, aligning with what the person wants to achieve. This client-centered approach is not about prescribing a fixed set of exercises; it is about coaching a person to experiment with different ways of doing things, to practice tasks in meaningful contexts, and to reflect on what works. Consider the rehabilitation needs of an adult dealing with chronic health issues such as obesity. The OT might guide the client to reframe daily routines so that health-promoting activities become natural parts of life rather than burdensome chores. They would help the person re-engage in the activities that matter—cooking, shopping, taking care of personal hygiene—while weaving in small, sustainable changes to behavior, such as meal planning, mindful snacking, or short, consistent movement.
A core strength of occupational therapy in adult rehabilitation is the emphasis on meaningful activities. The client’s life is not segmented into therapy sessions but into ongoing participation in work, family roles, and community life. The OT helps translate clinical goals into real-world practice. This translation often involves breaking down complex tasks into approachable steps, then gradually layering on complexity as confidence grows. A patient recovering from a hand injury, for example, learns not only to regain grip strength but to perform the precise micro-skills required to button a shirt, open a door, or handle utensils with ease. A person returning to work after a back injury might practice a sequence of movements that protect the spine, adapt work tasks to current capability, and manage the psychosocial aspects of returning to a professional role. The beauty of this approach is its versatility: the same principles apply whether the setting is a cozy kitchen at home, a bustling office, or a rehabilitation clinic.
In the broader landscape of rehabilitation, the alignment between occupational therapy and other health disciplines is essential. Interdisciplinary teams bring together different lenses—physiotherapy focusing on movement or gait, speech-language pathology guiding communication and swallowing, psychology addressing mood and cognitive strategies, and social work supporting access to resources and social determinants of health. The collaboration is not a backdrop but a dynamic engine. It requires transparent communication, mutual respect for each profession’s expertise, and a shared commitment to the client’s goals. For adults who are navigating multiple health challenges, this coordinated care grows easier when each professional understands how the others view a problem and how their interventions complement one another. The value of such collaboration is evident when a patient who has suffered a stroke begins to relearn skills at home, with the OT coaching daily activities, the PT guiding mobility, and the speech therapist reinforcing communication strategies that support social participation.
In rehabilitation, environments are not passively endured but actively transformed. Ot’s work often includes evaluating the home, workplace, and community settings to identify barriers to independence and safety. They may suggest simple rearrangements—reducing clutter, installing grab bars, reorganizing a kitchen for safety and efficiency, or designing a workstation that minimizes repetitive strain. Environmental modifications extend beyond physical space to include social and cultural contexts. An OT understands how family dynamics, transportation access, and community resources influence a person’s ability to participate in daily life. They may connect clients with supportive services, train caregivers, or help individuals advocate for themselves in healthcare or workplace settings. This integrative stance recognizes that disability or impairment is not only a medical condition but a lived experience shaped by a person’s rhythms, routines, and the supports available to them.
The role of motivation and empowerment in adult rehabilitation cannot be overstated. OTs employ motivational interviewing, goal setting, and collaborative problem-solving to foster a sense of agency. When a person sees tangible progress—an easier morning routine, a restored ability to cook a family meal, a step toward returning to work—the sense of possibility expands. This growth is not merely about physical function; it is about self-efficacy—the belief that one can influence outcomes in the face of adversity. The process honors the person’s values and life story. An OT will ask about what does a good day look like for the client, what small victory would change the day’s mood, and what barriers felt most insurmountable last week. As progress unfolds, the client’s roles—mother or father, employee, caregiver, partner—reconfigure around a new balance of capability and the demands of daily life. The OT remains a facilitator of this balance, guiding while stepping back to let the person lead.
The specific example of obesity management in adults illustrates how rehabilitation extends beyond the rehabilitation clinic into everyday life. Here, occupational therapy is not about a single diet plan or exercise prescription alone; it is about crafting sustainable routines that support healthier choices within the constraints and preferences of the client. The therapist may map out a day’s schedule to highlight opportunities for movement, meal preparation, and social connections that reinforce healthful habits. They teach skills in planning and prioritization, so healthy meals become the default rather than the exception. They may simulate grocery shopping to practice budgeting and reading nutrition labels, or design kitchen workflows that reduce fatigue and confusion. Importantly, they also address psychosocial factors—stress management, sleep quality, and emotional eating—that often derail even well-intentioned plans. This holistic approach reflects the reality that obesity is a complex, multifactorial condition whose management requires more than willpower; it needs a structured, compassionate strategy embedded in everyday life.
The effectiveness of occupational therapy in adult rehabilitation is supported by ongoing research across diverse health systems, including those that present unique challenges and opportunities. In some contexts, investigators are examining how OT programs can integrate more robustly into public health strategies, recognizing that improving daily function has ripple effects on community participation, employment, and social inclusion. Studies in different settings emphasize client-centered care, tailored interventions, and measurable outcomes such as independence in activities of daily living, safety at home, and quality of life. Within the scope of obesity and related conditions, research highlights the potential for OT to influence long-term behavior change by aligning interventions with individuals’ routines, family dynamics, and environmental supports. The evidence base continues to grow, and with it the understanding that rehabilitation for adults is most effective when it is systematic, collaborative, and deeply connected to what matters most to the person.
Despite the strengths of this approach, practitioners encounter real-world barriers. Limited access to care, transportation challenges, financial constraints, or cultural beliefs about health and illness can impede progress. OTs respond with flexible service delivery models, such as home-based visits, telehealth check-ins, or community-based programs that bring rehabilitation into environments where the person already engages in meaningful activity. They also work to make interventions culturally responsive, respecting diverse values and traditions while helping clients envision how these values can coexist with health goals. The ultimate objective is not simply to restore a task but to reframe a life around what is possible and desirable, even amid ongoing health challenges. In this sense, rehabilitation becomes a process of durable change rather than a sprint toward a single milestone.
The phrase “who does occupational therapy work with” increasingly reads like a list of potential partners who, together, shape a rehabilitation journey that reflects real life. An adult who has experienced a serious fall may rely on the OT to redraw daily scripts, reconfigure the home environment, and reestablish routines that guarantee safety and independence. A patient adapting to a new neurological diagnosis may find in OT a steady guide who helps them navigate cognitive strategies, sensory processing, and coping skills to participate in work and family life. A person living with a chronic condition may discover that small, consistent adjustments in day-to-day routines—meal planning, sleep patterns, energy budgeting—create a cascade of positive changes over time. In all these scenarios, the OT’s work remains grounded in the belief that people are more than their impairment; they are capable of growth, resilience, and renewed engagement with life.
Interdisciplinary teamwork continues to shape how adults experience rehabilitation. For a client who is returning to work after injury, the OT might partner with a vocational counselor to align job demands with functional capacity, or with an employer to negotiate reasonable accommodations. If there are speech, cognitive, or psychosocial components to a client’s recovery, the OT coordinates with the appropriate specialists to ensure that strategies complement one another. The client becomes the center of a small ecosystem designed to support recovery across multiple domains: physical, cognitive, emotional, and social. This ecosystem is not static; it evolves as the client learns new skills, tests strategies in real-world settings, and discovers what feels sustainable. The narrative of rehabilitation, therefore, is not a linear return to a past level of function but a reimagined pattern of participation that honors current realities while safeguarding future independence.
One practical takeaway for readers considering occupational therapy as part of rehabilitation is to view the client-therapist relationship as a partnership built on curiosity, respect, and accountability. The therapist’s expertise lies in diagnosing limitations and modulating activities to promote success. The client’s expertise lies in knowing their own priorities, values, and timing. When these two forms of knowledge converge, the path to recovery becomes not just a program of exercises but a lived strategy for living well. This is why, even within the constraints of a medical system, OT practice remains flexible and imaginative, always seeking to translate clinical insights into tasks and routines that people want to perform daily.
To further explore how occupational therapists connect with other professionals and integrate into broader care plans, readers can look to resources that discuss cross-disciplinary collaboration and practice standards. For example, a detailed look at how occupational therapists collaborate with other health care professionals offers concrete illustrations of teamwork in action and helps illuminate the practical steps that turn shared goals into shared outcomes how-do-occupational-therapists-collaborate-with-other-healthcare-professionals/. This kind of collaboration ensures continuity of care as adults move through different settings, from hospital to home to community programs, maintaining momentum in rehabilitation and reducing the risk of regression.
In closing, the question of who occupational therapists work with in the rehabilitation milieu reveals a profession deeply connected to the everyday realities of adult life. OTs serve a spectrum of adults—from those rebuilding after trauma to those pursuing healthier living and greater independence in the face of chronic illness. They work inside a framework that honors the whole person: physical capacity, cognitive engagement, emotional resilience, social participation, and personal meaning. The chapter that follows will continue to unfold how these elements come together in different settings, revealing the shared threads that unify occupational therapy across ages and diagnoses while also celebrating the unique paths each person takes toward renewed participation in life. External resources and ongoing research remind us that the field is dynamic, continually refining methods to help adults live with dignity, purpose, and independence. For those seeking deeper context, a foundational external resource offers accessible guidance on adult occupational therapy practice and outcomes, underscoring the relevance of OT across health systems and communities: https://www.aota.org/Practice/Patients-Clients/Adults
Supporting Independence in Later Life: Occupational Therapy with Older Adults
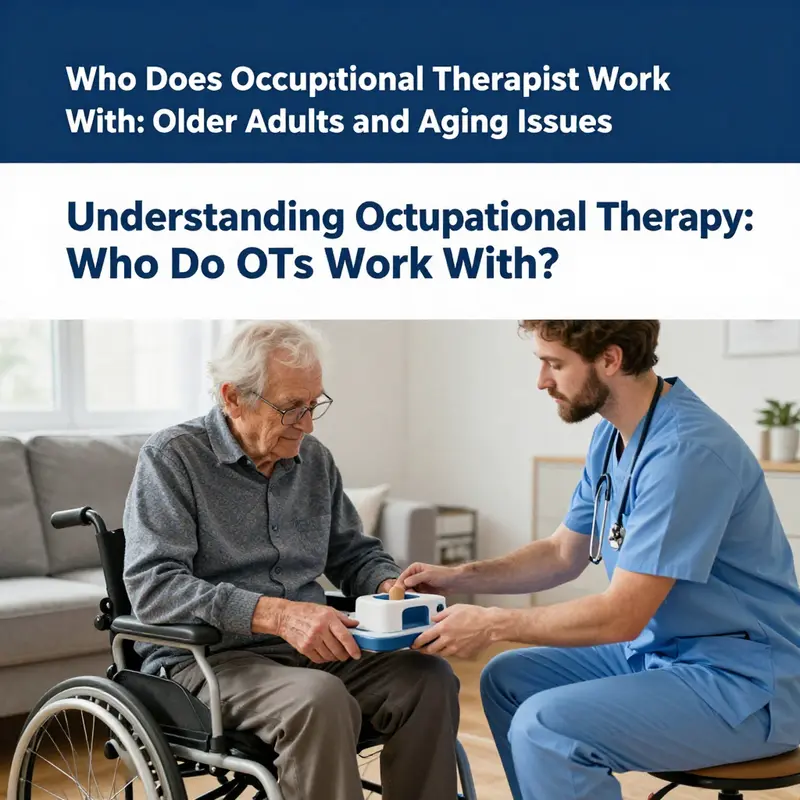
Across the arc of older adulthood, occupational therapists partner with older adults to preserve everyday function, safety, and meaning. They work in homes, clinics, and communities not to fix a single symptom but to support meaningful participation in daily life. The core aim is independence achieved through collaboration, adaptive strategies, and respect for personal goals. Aging introduces changes in strength, balance, memory, and routine; OT helps adapt tasks, environments, and tools so that daily life remains manageable and enjoyable.
Assessment begins with listening to the older adult’s priorities and then mapping abilities to real life tasks. The therapist considers the home layout, lighting, and accessibility; recommends modifications, assistive devices, or simple behavioral changes that reduce risk while preserving autonomy.
Caregivers and families are included as partners in care, with education and coaching to sustain routines without taking over. The evidence base for aging oriented OT emphasizes person-centered care, real-world outcomes, and holistic planning across physical, cognitive, and emotional domains.
Examples of meaningful activities include dressing, meal preparation, medication management, transportation, and social participation. The OT may introduce energy conservation, task simplification, and adaptive equipment (e.g., reachers, zipper pulls, shower chairs) to enable independence.
As aging continues to unfold, the OT remains a steady collaborator, adapting strategies as needs evolve and emphasizing dignity, safety, and choice. The result is ongoing participation in daily life — the hallmark of resilient aging.
Final thoughts
Occupational therapy is essential for enhancing the lives of diverse populations throughout different life stages. Children benefit from OTs through supported development, adults experience enhanced recovery and independence, and older adults gain assistance in navigating age-related challenges. Understanding the clientele of occupational therapists not only showcases the broader impact of this profession but also emphasizes the need for collaborative care in multidisciplinary teams, ensuring holistic support for individuals striving for better quality of life.