Cerebrovascular accidents (CVAs), commonly known as strokes, are a leading cause of long-term disability worldwide, affecting individuals physically, cognitively, and emotionally. Rehabilitation is critical for restoring function and improving the quality of life for stroke survivors. Occupational therapy plays an essential role in this rehabilitation process, focusing on helping individuals regain their ability to engage in daily activities. This article delves into the multifaceted role of occupational therapy in CVA rehabilitation, encompassing intervention strategies, cognitive function management, and patient-centered approaches. Each chapter will illuminate the significance of occupational therapy in helping stroke survivors reintegrate into their communities, ultimately enhancing their autonomy and quality of life.
Rebuilding Daily Life: How Occupational Therapy Drives CVA Recovery and Return to Function

Rebuilding Daily Life: How Occupational Therapy Drives CVA Recovery and Return to Function
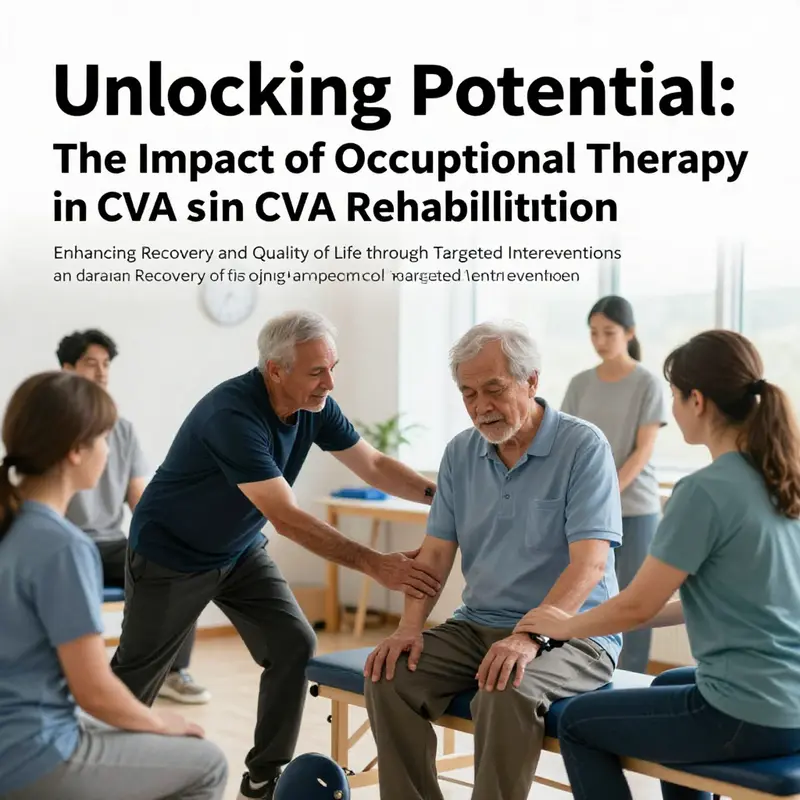
Occupational therapy (OT) sits at the heart of post-stroke rehabilitation because it translates clinical gains into real-life independence. After a cerebrovascular accident (CVA), patients often face a complex mix of motor deficits, sensory loss, cognitive change, and emotional shifts. These impairments do not occur in isolation; they interact to limit a person’s ability to perform meaningful activities. Occupational therapists begin by asking a simple but powerful question: what activities matter most to this person? The answer becomes the organizing principle for treatment. Rather than focusing solely on isolated body functions, OT targets the tasks, routines, and roles that define daily living. This focus gives rehabilitation direction and meaning and accelerates functional recovery.
Assessment in OT goes far beyond measuring muscle strength or joint range. Therapists conduct a holistic appraisal that captures physical abilities, cognitive skills, sensory perception, emotional state, and the environment where tasks occur. Observing a patient dressing, preparing a meal, or managing medications reveals breakdowns that standardized tests may miss. Assessments identify which steps in a task are problematic, whether the difficulty stems from impaired sequencing, limited reach, poor hand control, or safety concerns. They also highlight preserved skills that can be used as the basis for compensation and adaptation. This individualized understanding allows therapists to design interventions tailored to specific goals, preferences, and contexts.
Intervention strategies are diverse but unified by a practical aim: restore the capacity to participate in daily occupations. To achieve this, therapists blend restorative and adaptive approaches. Restorative methods aim to improve underlying impairments through graded practice, neuromuscular re-education, and therapeutic modalities. Exercises address range of motion, strength, coordination, and fine motor control in ways that are meaningful to the patient. For example, practicing the specific grasp patterns needed to hold a toothbrush integrates strength training with a real-world task. Therapists also use techniques such as task-specific training and constraint-induced movement therapy to promote use of an affected limb and encourage neuroplastic change.
Adaptive strategies accept that some impairments may persist and emphasize changing how tasks are done or modifying the environment. Task modification breaks activities into manageable steps, sequences tasks to reduce cognitive load, or introduces errorless learning for safety. Environmental adaptations remove barriers and reduce risk. Simple changes, such as reorganizing a kitchen so frequently used items are within reach, can restore an individual’s ability to prepare a snack. Recommendations may include grab bars, raised toilet seats, non-slip mats, and improved lighting. Where necessary, therapists train patients and caregivers in safe transfer techniques and fall prevention.
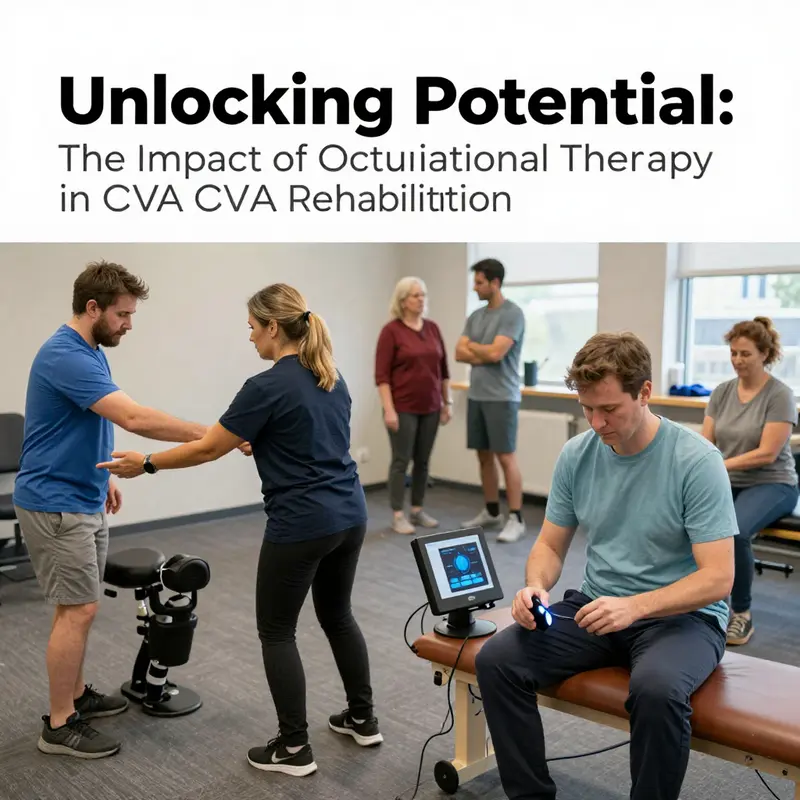
Assistive technology is another pillar of OT practice. Devices range from low-tech adaptive utensils and dressing aids to complex electronic aids that support memory and sequencing. Wheelchairs, orthoses, and splints maintain proper alignment and prevent contractures. More advanced options, including electronic reminders and voice-activated controls, can bypass cognitive limitations to support independence. Crucially, therapists evaluate not just device suitability but how the device fits into the person’s routines and environment. Successful adoption depends on usability, acceptability, and training.
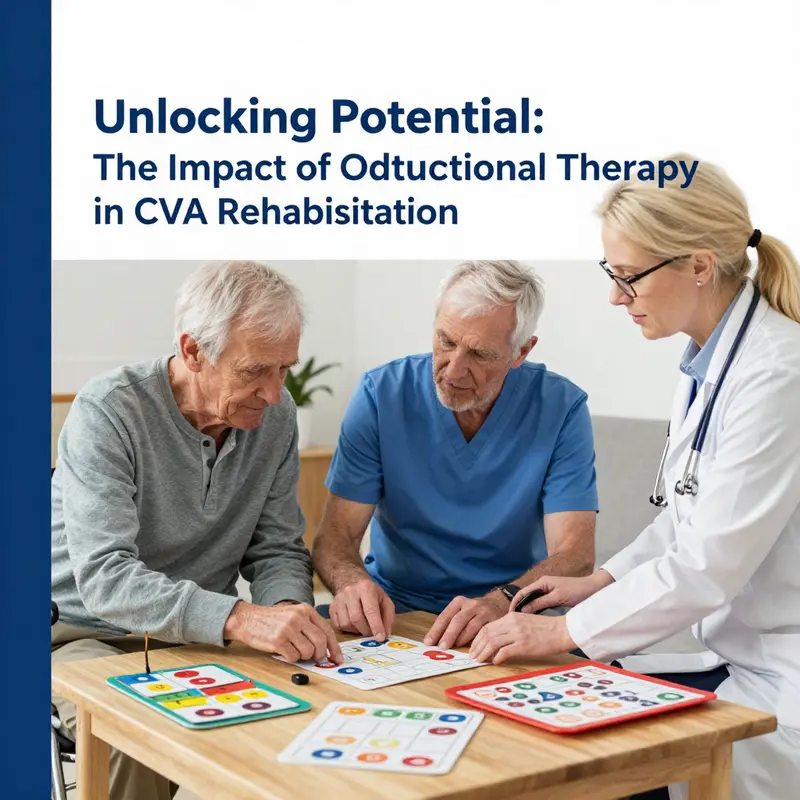
Cognitive rehabilitation is integral because cognitive deficits often limit progress in other domains. Memory difficulties, poor attention, slowed processing, and impaired executive function compromise the ability to learn new strategies and follow multi-step tasks. Occupational therapists apply cognitive training embedded within meaningful activities. Instead of isolated paper-and-pencil exercises, therapists design tasks such as preparing a simple recipe, managing a weekly medication box, or planning a short shopping trip. These activities require memory, planning, problem-solving, and flexible thinking. Therapists use graded cues and errorless learning to build success, then progressively reduce support to encourage independent performance. Strategies such as external aids, checklists, and structured routines become long-term supports when full cognitive recovery is unlikely.
Physical modalities and hands-on techniques remain important. Therapists may incorporate manual therapy to address soft tissue restrictions and joint mobility. Modalities including electrical stimulation, ultrasound, and therapeutic ultrasound can complement active training by reducing pain or facilitating muscle activation. Water-based therapy offers a low-impact environment for practicing balance and gait. Emerging technologies like biofeedback and virtual reality provide objective feedback and immersive practice, which can enhance motor learning. The choice of modality is always guided by functional goals rather than the modality itself.
Equally critical is the role of patient and caregiver education. Stroke survivors and their families must understand the nature of impairments, realistic expectations for recovery, and strategies to manage daily life. Education covers safe mobility, energy conservation, skin care for affected limbs, and how to structure a daily routine that promotes recovery. Therapists teach problem-solving skills and how to set incremental, achievable goals. These skills empower patients to take an active role in rehabilitation and support long-term self-management.
Return to community and work is a central OT objective, and interventions are crafted with that end in mind. Community reintegration includes social participation, transportation, and leisure pursuits. Therapists address barriers to these activities by improving functional capacity, recommending environmental changes, and coaching on compensatory strategies. For work re-entry, OT conducts job task analysis, identifying physical and cognitive demands of the role. Therapists collaborate with vocational specialists to adapt job tasks, propose graded return schedules, or suggest workplace modifications. This targeted, occupation-centered approach enhances the likelihood of sustainable return to employment.
Emotional and psychosocial factors shape recovery trajectories, and OT addresses them within activity-based contexts. Loss of role, reduced self-efficacy, and social isolation erode motivation. Therapists use meaningful activities to rebuild confidence and a sense of purpose. Group therapy and community-based programs promote social engagement and peer support. Interventions that incorporate meaningful roles—such as volunteering or mentoring—can restore identity and increase participation.
Interdisciplinary collaboration multiplies the impact of OT. Occupational therapists regularly coordinate with physiotherapists, speech-language pathologists, neurologists, nurses, social workers, and vocational counselors. This teamwork ensures that mobility, communication, cognition, and medical management align with functional goals. For instance, a physiotherapist may focus on gait training while the occupational therapist works on community mobility and ADL (activities of daily living) tasks. Joint goal-setting fosters coherent care plans and reduces redundant or contradictory therapies.
Evidence supports the value of individualized, problem-oriented OT approaches in improving outcomes after stroke. Tailoring interventions to the person’s priorities yields better engagement and more meaningful gains. Studies show that OT contributes to improved independence in self-care, better cognitive performance in everyday tasks, and enhanced quality of life. Integrating complementary practices, such as yoga or mindfulness, may further support physical flexibility and emotional resilience when aligned with patient goals.
Measurement and goal setting are practical tools that guide therapy and document progress. Therapists use both performance-based measures and patient-reported outcomes to track change. Goals are framed in behavioral terms, with clear criteria for success and timelines. This structured approach increases accountability and allows adjustments as recovery unfolds.
Long-term recovery after CVA often extends beyond formal rehabilitation. Occupational therapists prepare patients for this reality by fostering habits that continue improvement. Home programs, community therapy options, and access to adaptive equipment support sustained gains. Therapists also coach on strategies to prevent secondary complications, such as shoulder subluxation, contractures, or deconditioning.
Finally, cultural and personal context matters. Occupational therapists approach care with sensitivity to cultural values, personal roles, and socioeconomic constraints. Interventions are practical and respectful of the patient’s life circumstances. This person-centered stance helps ensure that recommendations are feasible and relevant.
Occupational therapy turns clinical knowledge about stroke into practical skills and environmental solutions that matter in daily life. By linking impairment-level interventions with task-oriented practice, environmental adaptation, cognitive support, and psychosocial care, OT creates a coherent path from hospital to home. The result is not merely recovery of movement but restoration of roles, routines, and participation. For detailed evidence-based guidance on occupational therapy in stroke rehabilitation, see this comprehensive resource:
Occupational Therapy for Stroke Rehabilitation | Springer Nature: https://www.springernature.com/gp/book/9783030524169
For further reading on clinical approaches tailored to stroke survivors, explore this practical overview of occupational therapy for CVA patients: occupational therapy for CVA patients.
null
null
Rebuilding the Mind: Cognitive Function in CVA Rehabilitation Through Occupational Therapy
Cognitive function after a cerebrovascular accident is not a peripheral concern; it is the fiber that determines whether a patient can translate physical recovery into real participation in daily life. In the arc of CVA rehabilitation, occupational therapy sits at the intersection of body and mind, linking the restoration of motor skills with the recovery of thinking, planning, and reasoning. The primary aim is not to restore cognitive capacity in a vacuum but to translate it into practical competence for activities of daily living, independence, and, crucially, the ability to return to work and social roles. This integration reflects a deep understanding that cognitive processes such as attention, memory, and executive function shape every routine from dressing to budgeting, from medication management to scheduling, and from meal preparation to navigating public transport. The chapter that follows outlines how cognitive function management is embedded within an OT framework, how therapists assess and treat cognitive impairments, and how they adapt communities and environments to support recovered function. It also connects the everyday work of OT with the broader evidence base that supports cognitive-focused rehabilitation as a crucial driver of outcomes after stroke, including the potential for meaningful work reengagement and enhanced quality of life. The path from impairment to independence is rarely linear, but the trajectory can be guided through deliberate, patient-centered strategies that weave cognitive training into the fabric of daily routines rather than isolating it as a theoretical exercise. A foundational premise is that cognition and daily activity are reciprocal; improvements in one domain reinforce the other, creating a positive feedback loop toward greater autonomy and confidence.
A comprehensive assessment lies at the heart of cognitive function management. Occupational therapists begin with a thorough appraisal of cognitive abilities that often underlie functional performance: attention and processing speed, memory—both short-term and working memory—executive functions such as planning and inhibition, and problem-solving skills. These domains are not isolated compartments but interacting systems that together determine a person’s ability to follow a shopping list, manage a prescription regime, or adapt to a changing home environment. The assessment process is twofold: it identifies strengths to build on and deficits to target, and it gauges how cognitive limitations interact with physical limitations, sensory changes, fatigue, mood, and motivation. This nuanced portrait informs a restorative and remedial approach known as cognitive remediation. Through this lens, therapists design individualized intervention plans that blend restorative exercises aimed at recovering cognitive processes with compensatory strategies intended to optimize functioning when recovery plateaus occur. The emphasis remains deeply functional; tasks are chosen and adapted to reflect the patient’s daily life and goals, ensuring relevance and engagement. In practice, this means that a session might pair a structured attention exercise with a real-world task such as following a recipe or managing a small budget, thereby anchoring cognitive work in meaningful outcomes. The restorative elements are not abstract drills but thoughtfully scaffolded activities that slowly increase cognitive demands while preserving a sense of mastery and control. A memory drill, for instance, might be embedded within a cooking task, or a planning exercise might be framed as preparing for a week’s worth of meals while simultaneously organizing a calendar and reminders for appointments.
The interventions that OT practitioners employ to support cognitive function are diverse yet tightly coordinated. Structured exercises to expand attention spans and improve sustained focus are combined with memory training techniques that emphasize encoding, retrieval, and real-life application. Therapists may introduce task-specific practice to strengthen executive functioning, such as multi-step problem solving that mirrors daily routines like preparing a grocery list, checking off items, and recalibrating plans if an unexpected interruption occurs. The aim is not merely to improve test scores but to elevate the patient’s ability to manage the complexities of daily life with greater independence. Real-life simulations play a pivotal role here. Therapists guide patients through activities that resemble real-world scenarios, such as handling finances, following multi-step instructions for a home project, or planning meals with limited time and resources. These simulations are carefully designed to be challenging yet achievable, promoting a sense of progress and agency. The cognitive work is not isolated carried out in a vacuum; it is embedded within an ongoing cycle of practice, feedback, and adjustment that reinforces learning and generalization to new contexts. Importantly, the approach respects individual differences in cognitive profiles, enabling a tailored mix of restorative exercises and compensatory strategies that align with each person’s unique goals and daily routines.
An essential dimension of cognitive function management is environmental adaptation. Occupational therapists recognize that cognitive deficits do not occur in a vacuum but are shaped by the environments in which a person lives, works, and interacts. Simplifying tasks, arranging spaces to reduce cognitive load, and providing reliable visual cues can dramatically reduce errors and frustration. Therapists may reorganize a kitchen or bathroom to create logical, clearly marked sequences that support safe, independent use. They deploy simple reminders, checklists, and organized routines to minimize forgetting and protect autonomy. In addition, the use of assistive technologies—ranging from straightforward calendars and alarms to more advanced reminder systems—can help patients manage time, remember appointments, and maintain task sequences. Environmental modifications extend beyond the home. In the workplace, therapists collaborate with employers to design accommodations that enable a stroke survivor to re-enter work with confidence. Job tasks may be broken down into steps, with built-in prompts and consistent routines that reduce cognitive overload. This holistic perspective—combining cognitive training with practical environmental supports—enhances the likelihood that gains in cognitive function translate into durable independence in everyday life and continued participation in meaningful roles.
The evidence base supporting cognitive-focused occupational therapy has grown robustly in recent years. A Cochrane Review by Gibson and colleagues in 2022 underscores that occupational therapy can significantly improve functional performance in everyday activities and contribute to cognitive recovery after stroke. The review emphasizes that the benefits are most pronounced when cognitive-focused OT is delivered consistently and tailored to individual needs, reinforcing the principle that personalized care drives better outcomes. This evidence aligns with clinical practice that prioritizes patient-centered goals, acknowledges the heterogeneity of cognitive deficits after CVA, and integrates cognitive training within the fabric of daily living rather than in isolated sessions. It also speaks to the essential partnership between cognitive improvement and environmental support, illustrating that gains in attention or memory are most meaningful when accompanied by practical strategies that enable safe, independent performance in home and community settings. In the broader landscape of rehabilitation, this evidence supports a model in which cognitive remediation is not an optional add-on but a core component of a comprehensive OT program that seeks to restore autonomy and social participation.
To translate evidence into care, many rehabilitation centers emphasize the critical collaboration between occupational therapists and other professionals. Cognitive recovery after stroke is influenced by mood, fatigue, language abilities, and physical function; thus an interdisciplinary team approach ensures that cognitive training is integrated with speech and language therapy, physical therapy, neuropsychology, and social work. Such collaboration helps align cognitive goals with broader rehab objectives, including motor recovery and psychosocial adjustment. It also supports a proactive approach to prognosis; OT clinicians often provide informed estimates about potential cognitive recovery trajectories based on initial assessments, progress over time, and engagement with therapy. This prognostic insight can guide families and caregivers in planning for home safety, long-term supports, and community reintegration, reducing uncertainty and fostering a more confident path forward. The role of the occupational therapist in this ecosystem is to act as a cognitive and functional architect, designing a plan that respects patient values while coordinating with the team to optimize every opportunity for relearning and independence.
Return to work remains a central and highly meaningful aim for many patients who sustain cognitive impairments after CVA. OT practitioners recognize that cognitive demands in modern workplaces are substantial and varied, often requiring sustained attention, flexible problem solving, memory for procedures, and the ability to anticipate and adjust to changing conditions. Consequently, employment-focused rehabilitation becomes an opportunity to translate cognitive gains into vocational gains. Therapists work with patients to simulate workplace tasks, identify cognitive bottlenecks that impede job performance, and develop compensatory strategies and workplace accommodations that reduce cognitive load while preserving productivity. The process often includes collaboration with employers to craft role adjustments, training that emphasizes prioritization and time management, and coaching to sustain motivation and reduce anxiety associated with work demands. A well-designed cognitive rehabilitation plan can help patients return to previous employment or transition to new roles that align with their current capacities, thereby preserving financial independence and social identity.
The practical implications for patients and families are profound. When cognitive function is supported through OT, individuals experience more than improved task accuracy; they gain a sense of control, reduce dependency on others, and experience enhanced self-efficacy. This development often translates into more engaged participation in family life, better adherence to medical regimens, and a greater willingness to engage with community activities. Therapists acknowledge that recovery is not a one-size-fits-all path, and they remain attentive to fatigue, fluctuating cognitive performance, and the emotional toll of adjusting to post-stroke life. The most effective programs are those that weave cognitive training into the rhythm of daily life and maintain an ongoing dialogue with patients about goals, challenges, and progress. In this sense, cognitive function management in CVA rehabilitation is less about restoring a specific cognitive score and more about restoring a reliable pattern of adaptive behavior, enabling people to live with dignity and purpose.
Clinical practice also emphasizes education and empowerment for caregivers and families. Understanding the nature of cognitive changes helps caregivers respond with patience, structure, and consistent routines that support independence rather than inadvertently undermining it. Education may cover strategies to reduce cognitive load at home, such as simplifying decision-making, providing clear and timely prompts, and modeling problem-solving steps in a patient and respectful way. By aligning home environments with therapeutic strategies, families become active partners in cognitive rehabilitation, reinforcing gains made in therapy and creating a supportive ecosystem that promotes long-term success. The goal is not to return to an idealized pre-stroke state but to achieve a resilient, functional life in which cognitive limitations are managed rather than controlling every aspect of daily living.
As practitioners look to the future of cognitive function management in CVA rehabilitation, ongoing research and clinical innovation remain pivotal. The current evidence supports integrating cognitive remediation with environmental modification and real-life practice, but the field continues to explore how best to individualize interventions, how to optimize dosage and intensity, and how to leverage technology to support cognitive recovery. There is growing interest in multimodal approaches that combine cognitive training with physical exercise, sleep optimization, nutrition, and psychosocial support to create a holistic recovery ecosystem. In practice, this means that therapists will increasingly tailor interventions to each patient’s daily routines, social context, and personal goals, using iterative assessment to refine strategies as cognitive capabilities evolve. The ultimate measure of success is not only the restoration of cognitive functions but the patient’s sustained ability to navigate life with independence, confidence, and equitable access to work and community participation.
For practitioners and families seeking deeper grounding in the evidence and best practices, the literature offers robust resources on how occupational therapy supports cognitive health after stroke. A practical exploration of cognitive remediation in OT can be found in stroke-focused OT exercises and strategies, which illustrate how cognitive aims can be embedded into everyday activities such as meal planning, budgeting, and medication management. For a concise, evidence-based synthesis of the cognitive outcomes associated with occupational therapy after stroke, consult the Cochrane Review linked below. This resource provides a rigorous analysis of how tailored OT interventions influence functional independence and cognitive recovery, helping clinicians calibrate their approaches to align with established findings while remaining responsive to individual patient needs. Occupational Therapy Exercises for Stroke. In the broader discourse of rehabilitation science, continuing work on cognitive remediation and environmental adaptation promises to sharpen the precision of OT interventions and expand the possibilities for stroke survivors to reclaim their lives.
External resource: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD013973.pub2/full
Putting Patients Front and Center: Personalizing CVA Rehabilitation Through Occupational Therapy
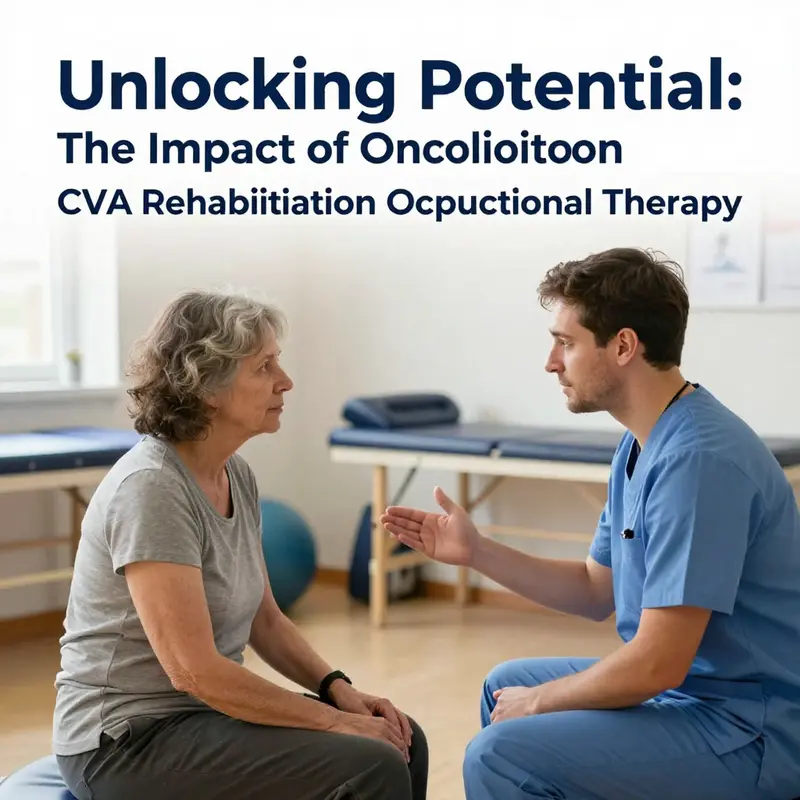
CVA rehabilitation, especially when guided by occupational therapy, is most effective not when therapists merely apply a standard sequence of exercises, but when care is tailored to the person who has lived with a cerebrovascular event. A patient-centered approach places the individual’s goals, values, everyday preferences, and life stories at the heart of planning and decision making. It reframes recovery from a clinical checklist into a lived experience that aligns with what matters most to the patient, whether that is dressing independently for work, managing the social demands of family life, or reclaiming a role in the community that extends beyond the home. In practice, this shift moves the care landscape away from a purely medical or task-based model toward a partnership where the patient is an active contributor to the rehabilitation journey. The result is care that not only targets physical recovery but also supports meaningful participation in daily life, which in turn fuels motivation, adherence, and sustainable outcomes. The occupational therapist becomes a guide who negotiates between clinical possibilities and personal aspirations, ensuring that every intervention, from mobility coaching to cognitive strategies, resonates with the patient’s sense of purpose and daily rhythm. The patient’s voice is not a one-off input at intake but a continuous compass that steers goal setting, measurement, and the pacing of therapeutic activities through the course of recovery. This orientation is particularly important in CVA rehabilitation, where the terrain of recovery can be uneven, and where small gains in function may unlock new social and vocational opportunities that patients deeply value. When care centers on the person, rehabilitation becomes a collaborative art, blending evidence-based techniques with the patient’s narrative to produce outcomes that feel sustainable and relevant in the long run. It is this fusion of clinical competence and personal meaning that defines the most impactful occupational therapy interventions after a stroke. In addition to restoring basic independence, patient-centered care supports patients in visualizing and pursuing a future that integrates physical capacity with everyday purpose, social connection, and work longevity. This chapter explores how occupational therapists operationalize patient-centeredness in CVA rehabilitation, describing the core components, the tools that illuminate patient priorities, and the ways in which care teams translate goals into concrete, adaptable plans that honor the patient’s life story while advancing functional recovery. The discussion draws on the growing body of evidence that person-centered care can improve the sensitivity of prognosis, the relevance of rehabilitation goals, and the overall trajectory of recovery. For clinicians, researchers, and students alike, embracing patient-centeredness means embracing a more nuanced, more humane, and ultimately more effective model of CVA rehabilitation that aligns clinical possibilities with human purposes, day by day, moment by moment. From the outset, this approach invites patients to reflect on what success looks like for them in the weeks, months, and years after stroke, and it invites care teams to listen, adjust, and respond with flexibility and empathy. It is through this ongoing dialogue that occupational therapy can help survivors reclaim not only independence in ADLs but also a sense of agency, resilience, and a pathway back to work and meaningful community participation.
Final thoughts
Occupational therapy is a cornerstone of CVA rehabilitation, providing essential support that enhances recovery and helps survivors regain independence. Through tailored intervention strategies that address both physical and cognitive challenges, occupational therapy facilitates a holistic healing process. By centering care around the individual, therapists not only improve functional abilities but also empower patients to reintegrate into their homes and communities. Understanding the comprehensive role of occupational therapy can inspire business owners to support innovative rehabilitation solutions that ultimately make a significant difference in the lives of stroke survivors.